February 2, 2024
Dear Interested Readers,
Is Healthcare Trapped In Its Own Groundhog Day Cycle?
My local newspaper has become a fertile field of thought and ideas for me. Last Monday, The Valley News, my local paper, had a front-page article that attracted my attention and got me thinking. It was entitled: “Health care bills aplenty: Abortion, circumcision, workforce among focus” written by a local journalist, Annmarie Timmins.
As the title suggests, many bills before the New Hampshire legislature have been proposed to improve some dysfunctional aspects or defects in our healthcare. The bills come from the right and the left and considering the almost fifty-fifty split in our legislature any bill is unlikely to pass unless it has broad bipartisan support. Our governor is a self-declared conservative but not a MAGA Republican. He was Nicky Haley’s biggest local supporter, and in the past, he has demonstrated that he is willing to veto any extremely repressive bill that might pass. He is also likely to veto any bill that adds expense to the state’s budget. I expect the end result will be that not much will change.
One of the bills is sponsored by Democratic Senator Cindy Rosenwald. She has a long history of progressive opinions representing Nashua in the New Hampshire House and more recently in our Senate. Senator Rosenwald proposes to spend 32 million dollars to add more healthcare workers and improve the education and credentialing of support staff. Some of the money may come from unspent COVID-19 money. The state spent $305 million last year in state and Medicaid dollars trying to improve access, but it was not enough to correct the state’s critical workforce shortage that impacts the system and its quality from the doctor’s office to the hospital and nursing homes.
In her article, Ms. Rimmons reports on Senator Rosenwald’s testimony before a Senate committee last week:
“It’s still very difficult to get a doctor’s appointment, which I can personally attest to, or get a hospital or a nursing home bed, get home care, mental health care, or substance use disorder treatment,” Rosenwald said. “So lack of adequate workforce has not only led to increased costs in this system as providers have had to pay enormous temporary staffing costs, but they’re also worrying implications that the quality of our fantastic health care system in New Hampshire is at risk.”
Senator Rosenwald is right to be very concerned. That statement was not a big surprise for me even though I know that New Hampshire was ranked third in the nation in access, affordability, and overall performance across a variety of metrics by the Commonwealth Fund in an article last June entitled “2023 Scorecard on State Health Care Performance.” I share Senator’s Rosenwald opinion based on my own experience and testimonies from my friends and neighbors. I worry that if New Hampshire is third out of fifty, and we have problems, there must be enormous problems in the other forty-seven states.
We have a penny-pinching legislature that functions under the state motto of “Live Free or Die.” The motto is attributed to a toast read in 1809 for General John Stark, the hero of the Battle of Bennington, who sent his written comments to a commemorative reunion of the famous battle that he could not attend because of illness. If you visit Bennington now, you will see a huge monument high on a hill, much like the one on Bunker Hill.
General Stark is not well known outside of New Hampshire, but there are bridges, highways, and high schools across this state that are named for him. His statue is one of the most impressive statues on the grounds of our statehouse. General Stark may have lifted the idea, if not the exact words, from mottos of the French Revolution or the words of Partick Henry. I sense that it is a wonderful concept that has been misapplied from the larger scope of human freedoms to the lesser subject of state taxes. The concept has been taken to a libertarian extreme as advocated by some people on the far right of the MAGA extremist movement called “free staters“, If they had their way, we would all be living down trails in the forest in log cabins surrounded by stone fences and armed with AR-15s, ready to defend ourselves from the ravages of “big government.” So much for that “aside” to explain our culture that Senator Rosenwald is up against as she advocates for progress here in the Granite State.
I believe in what Senator Rosenwald wants to do. My problem is that it is the equivalent of trying to dig a long wide trench with a spoon. She is doing the best she can, probably expects little success, and knows that if her bill did pass and the governor did not veto it, it would not solve our access issues.
What the article further reveals is the chaotic barrage of healthcare bills coming from both the right and the left at the state level. Some of the bills make sense and seek to expand Medicaid benefits and coverage at the state level. One of the sources of healthcare inequities in our country is that Medicaid eligibility and benefits are significantly controlled at the state level. Until the ACA was passed states were responsible for about half of the costs which justified their ability to control who was eligible in their state.
The ACA initially expanded eligibility for Medicaid and offered to ultimately pay 90% of the cost of the expansion. I never understood why such a great deal was initially refused mostly by Republican-controlled states. The Supreme Court has allowed states to refuse the expansion which New Hampshire and about half of the states did. New Hampshire finally signed on in 2014. It is my understanding that over the past few years, we have “conditionally” accepted the expansion, but the legislature has to “renew” the approval periodically. Last year North Carolina joined the list of states accepting the ACA expansion effective on December 1, 2023, which reduced the number of states now refusing the expansion to nine. I will leave it to you to guess which states still refuse, but a hint is that they are included in the graphic below as the ones with the lowest life expectancies and worst overall health outcomes as reported by the Commonwealth Fund last June.
There are other bills. Several relate to abortion. I hope that ultimately we have a statewide referendum that will permanently secure a woman’s control over her reproductive health. Ms. Timmons writes:
With Senate Bill 575, Sen. Debra Altschiller, a Portsmouth Democrat, is seeking to prohibit New Hampshire public officials from cooperating with efforts from outside the state to limit the state’s existing abortion access and access to contraception.
She has also sponsored a constitutional amendment, CACR 24, that would protect the right to “personal reproductive autonomy.”
[Lat update: On Thursday, after vigorous debate, all of the abortion-related bills from the left and the right were defeated. Those voting against the constitutional amendment claimed that there was no need since the current 24-week limit allowed abortions. There is still ambiguity in the interpretation, especially about late-term abortions for medical indications.]
I am sure that a similar potpourri of proposed legislation is brewing in most states. The deep divides in our country guarantee that without a different approach, we are destined to a back-and-forth process that makes very slow progress, if any, toward the Triple Aim or instituting the strategies for a better healthcare system for the twenty-first century, as outlined in 2001 in detail by the Institute of Medicine Committee on Quality of Health Care in America in Crossing the Quality Chasm: A New Health System For The 21st Century.
If one political party at either the national or state level gains a large enough majority to pass progressive healthcare policies then we can be sure that as soon as the other party gains power again much of the progress, if not all, will be reversed. It may not require a change in political control to undermine attempts to improve our system of care. Cases brought to the Supreme Court have done that even without the change of the party with majority control of Congress and the Presidency.
I would suggest that Congress recognize that the productive management and improvement of our healthcare system can not occur through a series of laws passed at the federal, state, and local levels. There is great variation in patient experience because of variations from state to state about what is covered and who pays. In a world where medicine will be practiced more and more across state lines facilitated by online access, it is increasingly clear that the current situation needs modification. During the COVID pandemic, I could access my PCP at Harvard Vanguard for online appointments from New Hampshire that were covered by our Blue Cross plan. Now that the rules have gone back to their pre-COVID status, I must take an unnecessary drive to Massachusetts to get much of my care.
‘We have a road map in Crossing the Quality Chasm that describes the “Big Harry Audacious Goal,” or “B-HAG,” the strategic objective that describes the components and standards of more effective, more efficient, more patient-centered, and less expensive care. We have literature about how to achieve strategic objectives. I would suggest approaching the wicked problem of our defective healthcare system with a process where Congress delegates control to a healthcare agency after clarifying that healthcare policy resides at the national level and is no longer in the domain of individual states. If “wicked problem” seems like slang to you it is a defined term:
A wicked problem is a problem that is difficult or impossible to solve because of incomplete, contradictory, and changing requirements that are often difficult to recognize. The use of the term “wicked” here has come to denote resistance to resolution, rather than evil. Another definition is “a problem whose social complexity means that it has no determinable stopping point”. Moreover, because of complex interdependencies, the effort to solve one aspect of a wicked problem may reveal or create other problems.
A wicked problem is a good description of healthcare in America as we approach the 2024 elections. What is going on in my state is a perfect example of spinning wheels and never getting out of the rut. Today is Groundhog Day. I would refer you to the wisdom of the Harold Ramis and Bill Murray movie of the same name. Something has to change if we are to get out of a repetitive cycle that goes nowhere, or if it does, it goes so slowly that past progress is lost by challenges that increase faster than feeble attempts at improvement. In the movie, Murray’s character realized that his interests needed to expand to include others if he was to ever get out of the cycle. We need to do the same thing to get out of our cycle of healthcare frustration.
I expressed almost the same thoughts in my letter of April 5, 2019. We need a new Healthcare system as advocated in Crossing the Quality Chasm. What we need even more is a way to implement strategic changes that carry everyone from the variation that we now have to a system that works well for everyone. We also need to realize that “we can’t get there from here.” In that 2019 letter, I referenced former Democratic Senate Majority Leader Tom Daschle’s 2008 book, Critical: What We Can Do About the Health-Care Crisis. Sadly, Daschle failed to report perks and income from lobbying, and his confirmation was blocked as Obama’s Secretary of Health and Human Services. His failure to become Obama’s healthcare czar was a huge loss in the struggle for the Triple Aim. His idea for a Federal Health Care Board, as described below, was great. It could easily be better, but it clarified a way to start to make lasting progress. In the introduction to his book, Daschle previews his idea which I think is still the best starting point on the path toward better healthcare in America. He writes:
In this book, I propose a Federal Health Board, modeled loosely on the Federal Reserve System, to do so. It would create a public framework for a largely private health-care delivery system. Its main job would be to develop the standards and structure for a health system that ensures accessible, affordable, and high-quality care. These standards would apply to federal health programs and contractors and serve as a model for private insurers. The federal government, through programs like Medicare, Medicaid, and the Veterans Health Administration, provides health care to roughly 100 million people. But these programs have disparate benefits, quality standards, and success in cost containment. If an independent board created a single set of standards for all of these programs, it would exert tremendous influence on every other provider and payer, even those in the private sector.
This idea is somewhat similar to The UK’s NHS, but it accepts the private ownership of our healthcare system. Competition and capitalism would continue to be a reality, but even Adam Smith, the patron saint of capitalism and free markets, knew that capitalism without some regulation was dysfunctional. Our stock market is regulated, our utilities are regulated, and our healthcare system could be shaped by a bipartisan appointed board that is empowered to protect and improve the cost, quality, and access to care of all Americans. The ACA attempted to do this, but its tools did not include a public option, nor was it truly universal. I shudder to think where we would be without it, but what it doesn’t provide is a pathway to an integrated system with a finance mechanism that doesn’t eliminate overuse use, underuse, and misuse of scarce resources. The board should be empowered to control the creation of new workforce members through innovations in clinical processes. Just as there is electricity, telephone service, and good roads in every corner of the country, we should also have adequate access to healthcare within reasonable distances.
The first step toward such a dramatic shift in our attempt to get a better system of care has to be the election of a majority in Congress that believes we need to do a better job and recognizes that new ideas are necessary. We almost did it in the 2008 election. Two more Democratic senators to balance the objections of independent Joe Lieberman and the death of Ted Kennedy would have given us a much stronger bill than we got with the compromises in the ACA. An even larger majority might have been able to create the governing agency that Daschle envisioned as the solution to the stagnation and erosion that persists in our healthcare policy and systems today. Maybe someday. Until then or some other better idea emerges, we will be like Bill Murray’s character who awakens every day to the same sorry experience.
If Dascle’s plan could be implemented, our job would be half done. Over the last quarter century, we have come to appreciate the powerful impact that the social determinants of health have on longevity and overall health. If you study the graph from the Commonwealth Fund earlier in this post it is easy to see that the worst outcomes come from states that have not paid as much attention to the systems of social service, housing, and education. Many of these states are committed to fossil fuel production and have resisted our nation’s attempts to address global warming. Donald Trump has frequently called global warming a hoax.
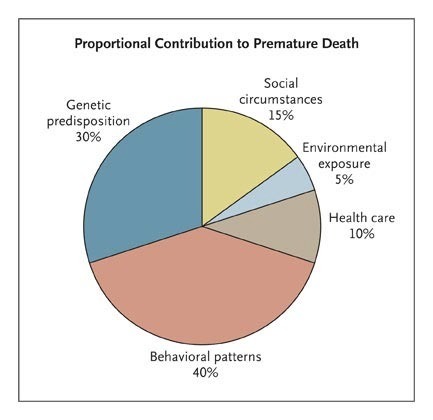
The reality that factors other than access to medical services are a significant determinant in longevity and overall health was well described in Steven Schroeder’s September 2007 paper in the New England Journal, “We Can Do Better — Improving the Health of the American People.” I have published a chart several times from his paper that emphasizes the importance of factors other than disease that influence health. Here it is again.
More recently this idea has been restated by some as: Your health is more influenced by your ZIP Code than your genetic code. Schroeder’s paper opened the eyes of some medical providers and institutions to the importance of the social determinants of health in the overall challenge of improving the health of the nation.
It takes time in medicine, often over a decade some say based on the experience with penicillin, for a new idea in medicine to become accepted enough to be integrated into common practice. It took an almost equally long time to convince practitioners that peptic ulcers were caused by an infection with Heliobacter pylori and not spicey foods and stress. There are always early adopters. I am very proud to serve on the President’s Advisory Committee at the Whittier Street Health Center in Roxbury where the CEO Frederica Williams has pursued an aggressive effort to address the social determinants of health since it was revealed over fifteen years ago that life expectancy of a resident in Roxbury was 59 years versus over 90 years less than two miles away in the ritzy Back Bay neighborhood of Boston. The Whittier Street website proudly says:
Championing equitable access to high-quality patient-focused care, social justice, and economic equity!
Perhaps someday we will accept what most European countries know, and what Whittier Street practices, which is that by improving the social determinants of health through investments in social services like housing, education, child care, and better transportation the health of the nation improves. We have a long way to go to escape our Groundhog Day frustrations. Moving healthcare policy creation as far away as possible from politics would be a good first step in the right direction.
Back To My Story: Lean and More
As we started our Lean journey with our Simpler consultants at Harvard Vanguard, I knew that it would be a slow process. The goal was to transform all of our operating systems including clinical practice sites and our management offices. It would be a huge, multiyear process to “roll out” a new philosophy to almost 5,000 employees in fourteen clinical sites and all of our management functions. I hoped that what happened at Harvard Vanguard would spill over to the other Atrius groups.
The first task at hand was to spread enthusiasm for Lean among the skeptics on the management team. The answer to that was to take them all to see Lean in action at Thedacare in Appleton, Wisconsin where John Toussaint gave us an introduction to Lean and an inspiring tour. A few members of the management team also visited Virginia Mason Medical Center in Seattle where Gary Kaplan had pulled off a very impressive introduction and development of Lean that involved taking many of his staff on excursions to Japan to have a hands-on experience working for a few days on the production floor of companies that were experienced in Lean production.
The majority of my team returned with true enthusiasm. Some expressed annoyance with Lean’s Japanese terms like Gemba, Kaizan, and Hoshin. I had expected that there would be a few who would still have some skepticism about doing something that would require a radical change in how they performed their responsibilities. Being a Lean manager requires going to where the work is done (the gemba), listening, asking leading questions, and giving new voice and responsibility to the people on the front line who do the work.
Being a Lean manager/ leader was quite different from their old jobs which were done while sitting in an office or attending meetings with other executives to create plans and pontificating about data that came from work they rarely observed. Some were open about their concerns, but most were willing to try Lean even if they were not so sure it would work for us. I should add that the majority of the board was enthusiastic and supportive, but as you might expect a few shared their skepticism in the form of probing questions that they put to me and the other members of the management team who were enthusiastic about giving Lean a try.
The other thing I did was try to sell Lean to our entire workforce through visits to our sites and the various management groups. This Friday letter was a valuable tool. In the letter, I described Lean philosophy and how I hoped that they would feel more empowered in their work. I told them about the successes at other healthcare organizations that were using Lean, and then I did an unusual thing. I offered that we would buy a copy of John Toussaint’s recently published story of Lean at Thedacare for anyone who would promise to read it. Within a week we had over 1400 promises to read On the Mend: Revolutionizing Healthcare to Save Lives and Transform the Industry. We bought the books. The unusual move was a good investment that jump-started awareness and enthusiasm across the organization.
Rolling out a new management process across a large organization requires a team of mentors and a detailed plan. The Simpler advisors led by Mike Hafer, the hands-on CEO, and Mike Chamberlain, the COO, were critical to our progress. They made frequent visits and became my good friends. On-site, I worked closely with Steve Matteson, Adam Ward, and my mentor John Gallagher. I eventually wrote a forward to Adam Ward’s book, Lean Design in Heathcare: A Journey to Improve Quality and Process of Care. There was a host of other Simpler consultants who were fabulous supports for me and effective teachers for our staff by leading them in successful RIEs, Rapid Improvement Events (Kaizen), that stimulated staff with hands-on experience. Simultaneously, while helping us teach our staff they were helping us develop what would be our own internal team.
A Lean transformation was a challenge that we could not have successfully accomplished without the experienced help of Simpler. Simpler had supported John Toussaint. They had advised Don Berwick at the IHI. They worked with Patty Gabow at Denver Health. They knew what they were doing, and they were good at transferring what they knew. I learned a lot as a frequent participant in RIEs, and from regularly attending the Friday morning reports delivered by front-line workers to the assembly of all the workgroups from the week and any others who were interested. It was inspiring to hear the presentations of the week’s progress through RIEs by the people who did the work.
Lean was a perfect fit for our key strategy of rescuing resources from waste and reinvesting those resources in clinical improvements. Before launching our Lean initiative our corporate employee satisfaction stats from a national resource were “fair to middling.” Not long after we began our “Lean journey” the scores shot up to the highest level at every site. Over the next few years, we were identified in several consecutive annual surveys by The Boston Globe as one of the best places to work in Eastern Massachusetts. Twice recently, while getting my care at one of our sites I had the joy of having a veteran employee tell me what an important, informative, and satisfying experience Lean had been for them.
By the time I retired, most of Simpler’s work was done. We were launched. We had our own internal Lean process improvement program and had harvested tens of millions of dollars for reinvestment in innovative care programs. Next week I will describe how we tried to influence other organizations in our local market and participated in the attempt to improve healthcare nationally.
No Shadows Here. It’s Been A Warm but Wonderful Winter
My local TV station in Manchester, the only TV station in New Hampshire, is proclaiming that when all the data is logged for this January it will probably be the warmest on record which will beat last January which also had that title. The forecast for the future has to be a continuing trend toward warmer and warmer winters because the progress we are making in reducing our use of fuels that produce carbon dioxide is not keeping up with the rapid acceleration of global warming.
Looks can be deceiving. When I look out the window it looks like a picture-perfect winter. The lake looks frozen, but the ice is thin as many people have discovered from chilly personal experiences. An almost nightly feature of the local news is a video of someone getting rescued after falling through the ice. The accident is often reported to have occurred because they were trying to rescue their dog which had first gone through the ice.
This year I am yet to see my first brave soul out on the lake ice fishing. Further adding to the illusion of a real winter is that there is more than a foot of snow on the ground, but intermittently the temp soars to over forty, for a few days which just creates a mess. That is what is predicted for this weekend. We are in a cycle of a week of frequent snow followed by a week of unseasonably warm weather. It’s freaky.
The picture in today’s header was taken a few weeks ago from the road up to the state park that is halfway up to the summit of Mount Kearsarge. In the valley below is Pleasant Lake which was way behind schedule and not completely frozen at that time. I wanted to get higher for a better picture, but the road was closed. A few weeks ago my son who has just become a father asked me if he could produce several headers for the letter before his son was born. By then we knew that the baby would be born early and his time to help me would be limited. That is why I was running around looking for pictures that might be appropriate to use over the next few weeks. If the picture had been taken this week, there would be more snow.
It will be interesting to see how February goes. I am eagerly awaiting the prediction of Punxsutawney Phil. I haven’t heard the result yet, but it has been pretty cloudy in these parts and I haven’t seen my shadow today. The drill is that if Phil sees his shadow, we will have six more weeks of winter. If he doesn’t see his shadow winter will end early. I predict an early end of winter.
Speaking of the new father and my new grandson, The baby is gaining weight and getting stronger but is still getting great care at Maine Medical Center. He will be two weeks old tomorrow. The original predictions were 4-6 weeks of hospital care, but I think he will go to his new home much sooner. I think that warm or cold weather this February won’t make much difference to me because I am focused on Forest. That’s the little fellow’s name. It is a name to grow into. At the moment he is still a little twig. But, he is a cute little twig with a world of potential.
I hope February 2024 will be a great month for you whether it is warm or cold where you are. I am planning several trips to Maine to see Forest. Remember that February is Black History Month and you probably have more to learn than many of our politicians want you to review. The link is a connection to programs on PBS this month.
Be well,
Gene



Steve, It is great to hear from you! You did live through all the history that I am trying to remember. Memory can be flawed, so please offer any corrections. I hope that our paths will cross sometime soon in Maine or New Hampshire. Young Forest, my grandson, is making great progress. We hope that he will be going home soon.
hello Gene- steve paskal here. not sure how i came across your “blog” but have enjoyed reading it the past few months.especially the history of the organization i have been part of for almost 40yrs, my retirement planned in june, if you are in portland at maine med my youngest daughter Margaret is a 3rd year med resident there- she will be joining a practice in Bath next fall, congrats on the new grandson ( i have 5 now – so wonderful). Plan to keep reading.steve