Some Articles You Should Read
The September 24th issue of the NEJM had two great articles in the “Perspectives” section on the new Medicare payment process, MACRA, the Medicare Access & CHIP Reauthorization Act of 2015. This new law that replaced the SGR, which many doctors never understood, was passed with large bipartisan majorities in both houses of congress. Since MACRA is not part of the much debated ACA, nor the target of any politician’s ire, it is likely to be with us for a long time. The universally hated SGR is gone and its bipartisan death is one of the more concrete expressions of the movement from volume to value, and it has occurred essentially out sight of the large majority of physicians.
“Leap of Faith — Medicare’s New Physician Payment System” by Jonathan Oberlander, Ph.D., and Miriam J. Laugesen, Ph.D. is the lead article in the September 24, 2015 NEJM and nicely describes the recent history of the SGR. The article is a very good prospective view of how the law will work and what the choices for doctors will be. As the phrase “leap of faith” implies the authors are not convinced that FFS payment is the reason that America’s healthcare is expensive or that this “next new” law will fix it. They are certain that this law does not signal the end of the political struggles associated with healthcare.
Meredith Rosenthal is a medical economist at Harvard and is the author of the article that follows “leap of faith”. Her viewpoint or “perspective” is a little different. In her terrific piece “Physician Payment after the SGR — The New Meritocracy”, she uses the same facts but comes to a somewhat different outlook. She notes that the SGR has been a major factor in physician compensation since the passage of the Balanced Budget Act of 1997 and describes MACRA not as a leap of faith, but as “an elegant compromise from a political point of view, crafted to end the tyranny of annual delays in physician-payment reductions but also to balance the need for public accountability against the profession’s interest in implementing a reasonable and predictable payment system”.
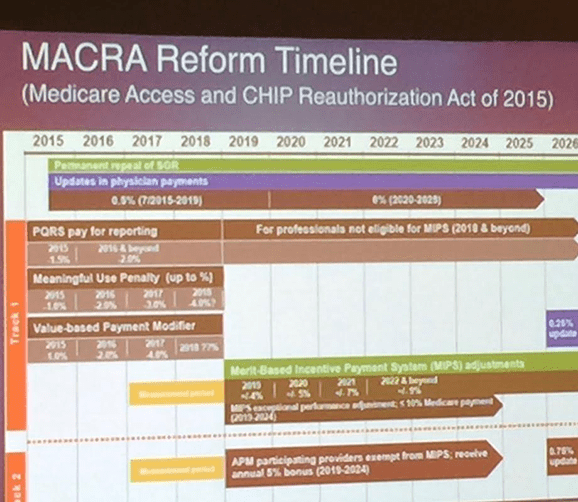
She gives us a very readable description and analysis of the hopeful philosophy behind the legislation as she explains the ins and outs of the new Merit-Based Incentive Payment System (MIPS) that will be phased in over the next five years and the other desireable option of alternative payment models (APMs) which are in essence ACOs. Neither article focuses much on the third choice offered by MACRA which is to accept small (0.5%) annual increases in FFS schedules that will continue until 2020 after which there will be no increase between 2020 and 2025. She focuses on the transformational parts of the law. I added the bolding for emphasis:
The replacement of the SGR with the MIPS marks a fundamental shift from setting annual fee levels on the basis of macroeconomic indicators (overall growth in Medicare spending relative to the sustainable growth rate) to relying on individual-physician- or group-level indicators of cost and quality. This change overcomes the “commons” problem that was inherent in physician incentives under the SGR. All physicians together were supposed to be accountable for the volume of services that drove Medicare spending, and all, regardless of their specialty or practice pattern, risked facing fee cuts when spending growth exceeded the target rate. That arrangement ensured that the SGR was only an accounting mechanism designed to force spending control after the fact (i.e., if price times quantity exceeds a given value, decrease price) rather than an incentive program — no individual physician had an incentive to reduce spending.
She points out that there will be choices for physicians. They can be viewed and judged as individuals or as a part of a practice or organization like an ACO. Describing the MIPS option she says that physicians and their organizations:
will be judged on the basis of four domains: quality of care, resource use, meaningful use of electronic health records, and participation in clinical practice improvement activities. Improvement in performance year over year will also be considered in physician assessments…The poorest performers will face fee cuts of 4% in 2019, 5% in 2020, 7% in 2021, and 9% in 2022.
Speaking of the third option, the APM’s, she logically concludes:
The new law should encourage participation in alternative payment models, including those associated with accountable care organizations and patient-centered medical homes. Professionals who receive a substantial share of their Medicare or all-payer clinical revenues through qualifying alternative payment models will receive a 5% bonus in each year from 2019 through 2024 and will be exempt from payment adjustment under the MIPS. This component of the law may well result in reaching an important tipping point in the take-up of voluntary alternative payment models in Medicare — and could potentially have a larger effect on value based purchasing than the MIPS itself. When it is implemented, the MIPS will become the largest physician pay-for-performance scheme in the world and the first to create a single value-based purchasing framework covering the full spectrum of physician specialties.
What becomes obvious to me is that MACRA, like the ACA is huge exercise in behavioral economics targeted at all levels of care delivery. Whether physicians are in solo practice, group practice, or employed by hospital or health systems, they are presented with choices that “nudge” them toward new finance models that are based on value and outcome. With the implementation of MACRA, we see the beginning of the final days of straight FFS. Perhaps after 2020 some FFS will continue as a mechanism to compensate some specialties for a while; but even those vestiges will occur within environments where quality and cost will be major determinants of the finance of the entire enterprise. In time it seems unlikely to me that those systems will use FFS payment for individual specialists without some connected penalties or incentives to help manage risk. Why should an organization accept payment for value and then turn around and compensate its employees or suppliers for volume?
How did this law sneak past physicians without much notice? Clearly the AMA understood and supported the move, but I have discovered few physicians who understood the potential future impact of MACRA on the way they will work and the way they are paid. Perhaps it will take a while for the importance of these changes to sink in for many who are still struggling the nuts and bolts of with how to move from a FFS mentality where success is measured on volume. Many physicians are unlikely to read or process what the NEJM published, but in a very succinct article their favorite “throwaway” journal Medical Economics says exactly the same things and points to the need that every physician has to begin to change the way they think about medical homes, ACOs, population medicine and the consideration of cost and patient satisfaction.
I would predict that over the next few years, as the sun sets on volume based reimbursement, many organizations will suddenly realize the need to quickly learn what they have avoided. Some may even consider what Lean may offer as they try to come up with survival strategies. They may even realize the benefits of focusing on the Triple Aim Plus One. Perhaps they will be concerned with patient service, managing waste out and quality into their processes rather than focusing purely on the objective of revenue generation.