June 30, 2023
Dear Interested Readers,
Where Does Your State Rank?
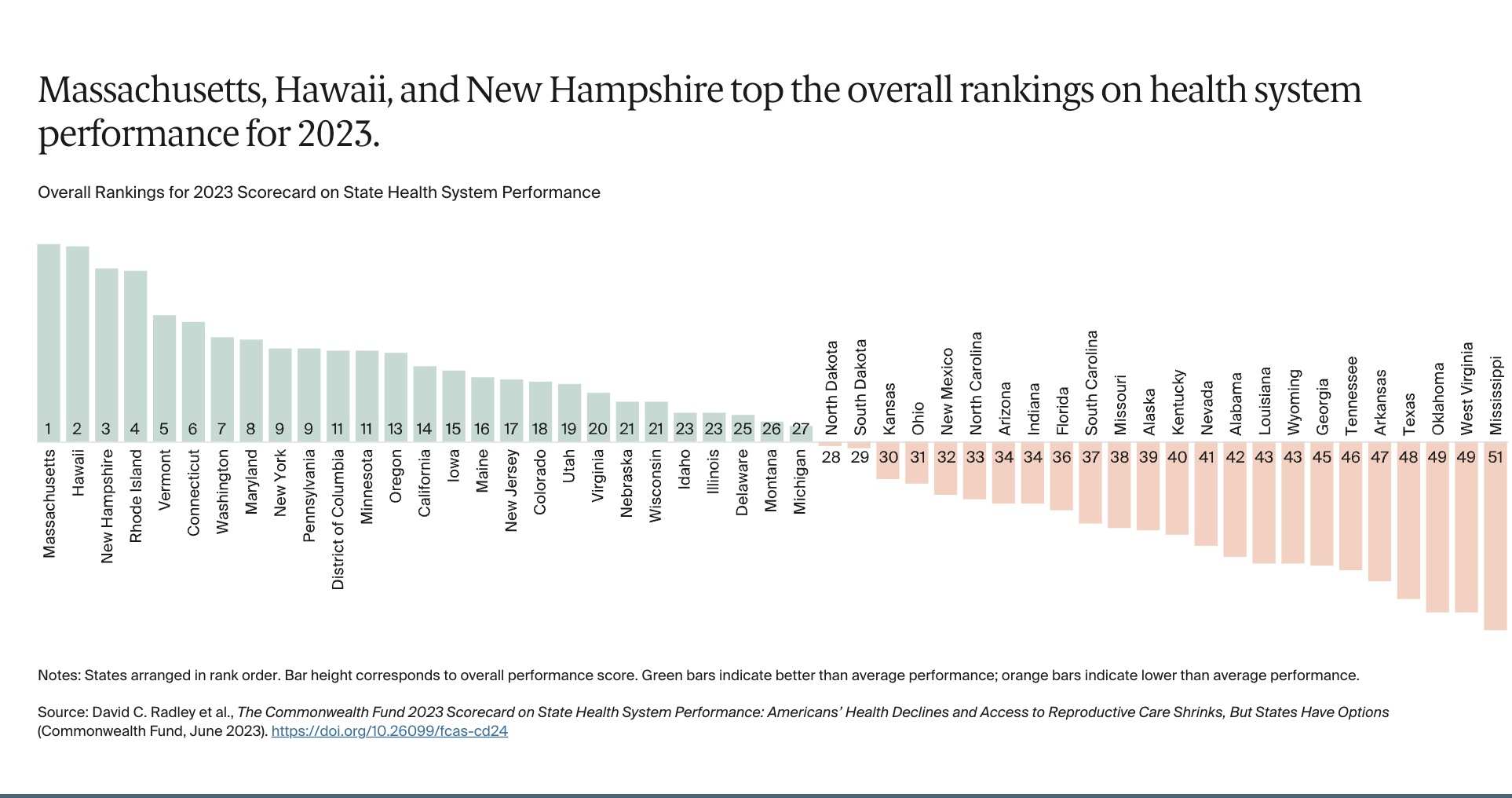
Every year The Commonwealth Fund ranks the healthcare in each state. This year’s rankings were published last week on June 22 in an article entitled “2023 Scorecard on State Health System Performance: Americans’ Health Declines and Access to Reproductive Care Shrinks, But States Have Options.” For your convenience, I have lifted their graphic presentation of the rankings.
My former home state, Massachusetts, is number one. The healthcare in Massachusetts is very good and over 98% of the population theoretically has access to care, but I expect it is still one of the most expensive states for care in the country despite the efforts of its statewide board, the Health Policy Commission, to control costs. I was somewhat surprised to see that Hawaii is number two. I wrote about healthcare in Hawaii and its problems with primary care back in 2019. It would be interesting to understand what they have done to improve their outcomes. My current state, New Hampshire is a surprising number three in the overall evaluation of over fifty parameters because it is very difficult to find a PCP here although I know that there are people working hard to change that reality, and Dartmouth Health has a focus on the community.
Little Rhode Island at number four is my wife’s home state, and brave little Vermont rounds out the top five. I am delighted that there have been effective efforts for improvement in Rhode Island. Those efforts have moved the little state up from seventh place in 2019 to fourth place in the current evaluation. In 2019 the Commonwealth Fund published an article that described what is happening in Rhode Island, I say that Vermont is brave because I believe no other state has tried harder to provide its citizens with a state-sponsored program of universal access with value-based reimbursement than Vermont. (There is also a Vermont Public Radio Podcast entitled “Brave Little State,”) I once wrote that the vision for Vermont was one statewide ACO. That is possible because the state’s population is less than 700,000. Massachusetts, Hawaii, New Hampshire, Rhode Island, and Vermont make the case for the fact that coordinated efforts to improve healthcare can make a difference. In each of the top five states, there have been effective statewide efforts that have made a difference. Would it not be great if some of the less successful states adopted the attitudes and efforts of these top five states?
My first question as I began to look at the Commonwealth Fund data was where do the ten states that continue to refuse the Medicaid expansion of the ACA rank? The strangest of the ten states for me is Wisconsin which is the home of some very good healthcare systems like Aurora Health, Gundersen Health, Beloit Health, Dean Health, and ThedaCare. Wisconsin has a divided government. In Wisconsin, statewide elections can produce Democratic winners, but the legislature is controlled by rural Republicans which is the probable explanation for the failure to adopt the Medicaid expansion when the largest city, Milwaukee has a large population that would benefit from the expansion of coverage. The other nine states that have continued to block the ACA’s expansion of Medicaid fall into the lower fifty percent where you might expect to find them: Kansas (30), Florida (36), South Carolina (37), Alabama (42), Wyoming (43), Georgia (45), Tennessee (46), Texas (48), and Mississippi (51). Yes, Mississippi (51) since the District of Columbia (11) was included in the analysis.
Many of the other original deniers of the Medicaid expansion of the ACA have seen the light, but perhaps their attitude about universal coverage and their slow adoption of the Medicaid expansion is reflected in their continuing below-average performance. West Virginia and Oklahoma are “tied” at number 49. West Virginia has a predominately Caucasian population and high levels of poverty that create problems with the social determinants of health, but its voters consistently vote against their own best interests despite the fact that they are the second highest per capita consuming state of federal aid. It amazes me that three of the five states that are most dependent on federal aid for the welfare of their citizens consistently elect senators and representatives who vote against and block the policies and programs on which their impoverished citizens depend. The top five recipients of federal aid are:
1: Alaska
2: West Virginia
3: Mississippi
4: Kentucky
5: New Mexico
Louisiana waited until 2016 to accept the Medicaid expansion. Perhaps that is why they weigh in at number 42. I know that it is not a certain correlation, but there is some evidence the 24 states, with the exception of Wisconsin, that originally did not want to expand their Medicaid programs, even though the federal government was going to assume 90% of the cost, are the same states that rank in the bottom half of the performance evaluation “based on 58 measures of health care access, quality, use of services, costs, health disparities, reproductive care/ women’s health, and health outcomes” done by The Commonwealth Fund. Beyond universal coverage, the other predictors of the quality of care are access to primary care and the level of attention to the social determinants of health.
Beyond the rankings, The Commonwealth Article made some overall observations about the outcomes for this last year that are worthy of notice. I have added some bolding to draw your attention to key points
- Deaths from COVID-19 — as well as premature, avoidable deaths from causes like drug overdoses, firearms, and certain treatable chronic conditions — rose dramatically during the first two years of the pandemic, lowering life expectancy across the United States.
- There was wide state variation on the Scorecard’s new measures of health outcomes and access to care for women, mothers, and infants. Maternal mortality and deaths related to substance use rose quickly among women of reproductive age during the pandemic — a particular concern given new state policies limiting reproductive care access.
- Temporary federal policies during the COVID-19 pandemic drove uninsured rates to record lows, with nearly all states realizing gains in health coverage. But some of those policies have ended, and high health costs still saddle millions of Americans with medical debt.
- There are ways the nation could improve health outcomes and lessen variation from state to state. Federal and state governments could: close the coverage gaps that remain and enroll uninsured people who are eligible for subsidized coverage; improve the cost protections of insurance plans; and lower barriers to reproductive health, preventive health, and behavioral health care, particularly for the most vulnerable.
There is no doubt that the entire nation has been under great stress from the pandemic and the economic and emotional stresses associated with the shuttering of non-essential businesses, the disruption of normal social interactions, and the impact on families from children being unable to go to school. The sum total of all the disruptions in care and in life led to a fall in life expectancy across all populations and all states from avoidable complications of chronic disease, mental health issues, and poor access to care. It has been said before, but the increased mortality disproportionately impacted the poor and minorities. What amazes me is that we can identify what happened and have plausible remedies that could be applied, but there has been little enthusiasm for retaining what did work during the pandemic or developing new policies that might make a difference going forward.
The report also identifies the increased deaths from firearms. A review of the state rankings suggests to me that the states with the poorest access to healthcare also have the greatest resistance to commonsense changes in access to firearms. The Commonwealth report calls specific attention to the states that had the greatest increases in preventable deaths.
All states experienced large increases in avoidable deaths between 2019 and 2021, leading to substantial declines in life expectancy across the U.S. Arizona, Louisiana, Mississippi, New Mexico, and Texas stand apart: each experienced more than a 35 percent increase in avoidable mortality rates over this period. Arizona’s rate jumped the largest percentage, by 45 percent.
The report is bold in its pronouncements. The report does not mince words about the egregious outcomes experienced by minorities during the pandemic. It seems to suggest that there is a correlation between controlling attitudes within a state and its healthcare outcomes and quality.
These disparities in outcomes have deep roots: the nation’s history of structural racism; generations of discriminatory state and federal policies around housing, education, and employment; health insurance policies that disproportionately disadvantage people of color; and well-documented variations in patient care quality by race and ethnicity. Together, these factors played a major role in many of the poor health outcomes seen across the U.S. both before and during the COVID-19 pandemic.
Unfortunately, it is discouraging for many of us that it seems that there have not been meaningful lessons learned from the pandemic. It seems that much of the progress that was made to improve access to care and address inequities in care during the pandemic has been quickly abandoned in the rush to “return to normal” in the immediate aftermath of the pandemic.
On Tuesday, Dr. Rochelle Walensky who is leaving her post as the Director of the CDC, published her concerns about our future as a function of the attention that we give to public health in an Opinion piece in The New York Times that deserves your attention. Her message was entitled “What I Need to Tell America Before I Leave the C.D.C.”
Dr. Walensky’s main message was that we can’t afford to neglect Public Health now that we have declared the pandemic is over, but it is obvious that she is afraid we will. The support that public health should be given is already being withdrawn which will make us as vulnerable to the next pandemic as were to the last one. She reminds us that the only uncertainty is when that pandemic will come, not if it will come. She writes:
Decades of underinvestment in public health rendered the United States ill prepared for a global pandemic…During the pandemic, the answer to these prevailing problems was a rapid infusion of money — resources that were swiftly withdrawn.
Not learning lessons, or ignoring lessons for political reasons seems inconsistent with our embrace of science and the vast expertise that allowed us to rapidly develop tests to identify infections and vaccines to reduce the mortality and morbidity of the virus. That we would demobilize our public health apparatus after what we experienced makes little sense. The Commonwealth Fund’s report expands its analysis of the impact of the pandemic on the current status of care in the country by focusing on how the pandemic exacerbated other issues that predisposed to bad outcomes and led to increased mortality from avoidable deaths. First on their list is the collection of mental health issues and substance abuse problems. They write:
Amid rising concerns over mental health and record-high deaths from suicide, alcohol use, and drug overdose, many Americans are struggling to get the behavioral health services they need. In addition to causing more than 1 million deaths, the COVID-19 pandemic also exacerbated mental and behavioral health issues for many Americans. The consequences have been dire: in 2021, for the first time, combined deaths from drug overdoses, alcohol, and suicide claimed upwards of 200,000 lives, some 50,000 more than the prepandemic high, in 2019.
Their next insight is the impact of the status of reproductive care and women’s health on outcomes.
State performance on reproductive care and women’s health varies widely across the country. Many of the states with the worst outcomes are now implementing or considering further restrictions on reproductive care, raising concerns about inequity in access and health outcomes.
This year’s Scorecard features a new domain of health system performance — Reproductive Care and Women’s Health — to rank states on health outcomes for women, mothers, and infants and access to important health care services. The 12 indicators it includes measure mortality, such as maternal and infant deaths; high-risk events, such as severe maternal morbidity and preterm births; and ability to get routine checkups, prenatal and postpartum care, and other vital services.
The Dobbs decision overturning the right to abortion has already had a negative impact on the metrics of quality in the states that have made it illegal or more difficult to access abortions. The report predicts that things will get worse.
Twenty-six states now have abortion restrictions in place following the Court’s ruling. These restrictions will not only reduce or eliminate access to abortion services, but they could also limit access to providers that offer important preventive health care like contraception and reproductive cancer screenings. Many of these reproductive health care providers are concerned they will no longer be able to deliver high-quality care, while others fear being criminalized for providing their patients with the full spectrum of reproductive services.
Women with low income, women of color, and women in rural communities will be especially impacted by these changes in health care access. They disproportionately live in those states that have enacted additional abortion restrictions, and they are often the ones to experience the most acute effects of any systemic failure or shortcoming.
This last week was the first anniversary of the Dobbs v. Jackson decision. An Axios article published last month described the healthcare challenges that have evolved since the decision. The article includes a map that shows the states where Republican-led legislatures are passing laws that threaten the health of all women.
As more bans go into effect, people seeking abortions have been forced to either travel hundreds of miles to another state that allows abortions or order abortion pills that are prescribed online and delivered through the mail.
However, state lawmakers have already cracked down on abortion medications and may seek to prosecute people who cross state lines to get an abortion.
The environment associated with the passage of these bills and the potential criminal penalties for doctors and organizations that provide abortions and reproductive health has already had profound effects on practice and outcomes. It is interesting to compare the Axios map with the graphic published by The Commonwealth Fund. If you do so you will see that New Mexico and Alaska are the only states in the lower twenty of the health outcome rankings where women have access to abortion. Both of those states have issues of poverty or large indigenous populations which may explain much of the overall performance that puts them in the lower tier of states in healthcare rankings. The Center For Reproductive Rights publishes a regularly updated map that shows the status of abortion in each state. When you use the map, just click on a state and the status of abortion rights will pop up.
The authors of the Commonwealth Fund report describe what will need to be done to improve the inequities in women’s health that have led to increased maternal and infant death rates:
To improve these outcomes, it will be critical to integrate the continuum of reproductive health services before, during, and after pregnancy with primary care, including preventive services like cancer screenings and behavioral health services like substance use treatment.
Unfortunately, shortages of maternal care providers are commonplace across the U.S.; some communities are even considered to be “maternity care deserts.” Other women don’t have insurance coverage or can’t find providers who accept their coverage.
The report includes extensive appendices that document what was measured, and allow a deeper dive in the differences in the status of care from state to state. Some of the differences that are then manifested in deaths are shocking. They report that 29% of pregnant women did not get first-term care in Texas or Florida compared to the best-performing state, Vermont, where only 11% of women were not seen during their first trimester.
”
Florida Governor DeSantis, a candidate for the Republican nomination for president, likes to say “Florida is where woke goes to die.” The data from the Commonwealth Fund suggests that “woke” is not the only thing that dies regularly in Florida. It is shocking that the maternal death rate in Florida where woke dies is four times higher than in California. There is a new manifestation of the “solid South.” The five worst-performing states in terms of maternal death rates that are even higher than in Florida are Arkansas, Alabama, Louisiana, Tennessee, and Mississippi. Again, Mississippi is the worst.
As we shake our heads in disbelief, the only logical question to ask is what can we do? The answers that the Commonwealth Fund offers are not new. You have read them here before, but until things improve you will read them again and again. It is a long “to-do” list. They begin by saying that there is room for improvement in every state and at the federal level. What concerns me is that compared to a decade ago when I retired there appears to be no sense of urgency at any level of government. I hope that some critical number of “woke” politicians will take it on as a challenge. We need to renew our enthusiasm for better health. Their list does not begin by suggesting that we throw away our current system of care in favor of some sort of federal “Medicare for All.” It envisions working within our current care model built on private employer-based insurance, Medicaid, Medicare, and a more fortified and supported ACA. Here is their very practical list:
- Expand the primary care workforce.
- Promote primary care and behavioral health integration.
- Increase treatment for behavioral health needs of children and adolescents.
- Increase access to addiction care.
- Expand comprehensive harm reduction policies.
- Develop community-based health care workforces focused on team care.
- Extend and provide support for evidence-based implementation of Medicaid’s postpartum coverage to 12 months.
- Promote policies, innovative payment models, and digital tools that support the continuum of reproductive health care — from family planning, abortion services, and maternity care to postpartum and well-woman care.
- Provide funding to community-based organizations focused on advancing maternal health outcomes and addressing racial equity.
- Expand and diversify the maternal and reproductive health workforce by investing in teams of physicians, midwives, doulas, community health workers, and maternity care coordinators.
- Invest in care models that support mothers with maternal mental health conditions and substance use disorders.
- Increase financial investments in social determinants of health that influence maternal health outcomes.
- Continue to prioritize the elimination of racial inequities in maternal health.
- Fill the Medicaid coverage gap.
- Permanently extend enhanced marketplace premium subsidies set to expire in 2025.
- Create a longer period of continuous Medicaid eligibility.
- Create an autoenrollment mechanism.
- Lower deductibles and out-of-pocket costs in marketplace plans.
- Lower health care cost growth.
- Protect consumers from being financially ruined by medical debt.
I don’t think the list is complete. There are many other changes that could be considered that would certainly lead to better outcomes and better health for every American, but just accomplishing a few of these recommendations would make a difference. I fear that things are in such a state of decline that no one or no group with the political power to make policies that could make a difference has the political will or the energy to take up the cause of better care.
There are cultural concerns that are creating a deeper divide and at least a third of voters lack any obvious concern for those who are excluded from the comforts of wealth. The other two-thirds of the electorate are so terrified of a return to MAGA politics that they have little energy left to discuss improvements in health care policy and not much is possible anyway as long as the House is controlled by those who seem to have no interest in improving the care of those who are less fortunate.
Other issues like the economy and the potential for expanding international conflicts deserve much attention and have supplanted healthcare improvement as a top political concern. I fear that global warming is a reality that can no longer be reversed, and now the issue is how will we deal with it as it worsens. The choice seems to be between being “woke” and active or being self-interested and dismissive of the evidence that we have some very challenging problems to face together.
It’s Been Raining Continually
I well remember my eighth-grade English teacher stressing the difference between continuous and continual. In case you missed that class, here is the difference. Continuous means “forming an unbroken whole; without interruption.” Continual means “frequently recurring.” According to scripture, Noah and his family and the animals he had loaded onto the Ark experienced forty days and forty nights of continuous rain. Here in New Hampshire we have had rain most days for the past two weeks and the forecast is for more, but it is continual which means that there are breaks in the deluge when I can get out on a walk. When I am lucky those walks are associated with continual breaks in the cloud cover and things look pretty nice as they did earlier this week when I took the bucolic picture of the very good-looking cows that I encounter on my walks.
We have a segregated cow population. Two weeks ago the header pictured the very handsome white cows on the Mount Sunapee side of the road. This week we are looking at the brown cows with white faces on the other side of the road. If I just look at the cows, the fields, and the stone walls I get a sense of what it might have been like around here one hundred and fifty years ago or earlier. This area was tough for farming because of its rocky soil and did not get populated until the late seventeen hundreds. What it did have was water power on its small streams and rivers that were flowing downhill and plenty of rocks to make fences to contain livestock. The result was farms that produced milk from cows and sheared sheep that produced wool for local mills to process. A little-known historical fact is that by 1840 there were 600,000 merino wool-producing sheep in New Hampshire. The stone walls were perfect for keeping those sheep in place.
All the roads that I walk are bounded by continual, there are breaks so not continuous, stone walls. My own two acres have stone walls that run through the woods indicating that the property was once clear-cut and valued not as a great place for a lakeside recreational home but rather it was a good place to graze livestock. I assume that the cows and sheep just wandered over to the lake whenever they were thirsty. I would like nothing better than to be able to time travel back for a few hours to see the scene that I can imagine in my mind’s eye as it really was.
Getting back to continuous versus continual, It appears that the South and Southwest are in the midst of continuous heat with a continual series of violent interruptions in the form of damaging hail and tornados. Our continual rain has been spiced with very loud thunder and occasional flashes of ominous lightning. What I haven’t seen is a rainbow. The lake is so high that the buoys where I moor my boats are being pulled underwater and the beach has disappeared into the lake. It is at times like this that I remind myself that when it comes to weather, “This too shall pass.” I wish that I could be just as certain about the decline in the quality of healthcare in America. I fear that when it comes to our health we have not seen the worst yet and that our journey has been, and will continue to be, a continuous decline.
One of the most enjoyable reads this year for me has been George Saunders’ very wonderful review of four stories from the great Russian writers of the nineteenth century. The book is entitled, “A Swim in a Pond in the Rain.” I highly recommend it for your summer reading list when you are relaxing at the beach or forced to stay inside because of the rain. I have taken the advice literally and don’t let a little rain keep me from my daily swim.
I am hoping that one of the breaks in our weather pattern will occur for the week of the Fourth and that wherever your plans take you, you will have a relaxing holiday experience with family and/or friends.
Be well,
Gene