It is always difficult to think about the future. Will it be more of the same, a great leap forward, or a big step backward? Can we see something inevitable on the horizon? Is there something that will be totally unexpected like 9/11 that leads to big surprises? As is true in Cormac McCarthy’s novel, The Road, many of the visions of the future in literature and film are post apocalyptic or “dystopian”. We seem to have had a hard time getting over our fears of a dark future after a nuclear holocaust or some other global disaster that sends us back to some future oriented facsimile of the dark ages. If we have made any progress in overcoming worries about a future that contains a nuclear disaster, perhaps we have transferred those worries to new concerns about terrorists, “global warming”, our uncertain global economy. At times it appears that healthcare professionals seem to act as if the future of healthcare will be dystopia.
Thinking about the future does not usually correspond to the laughs we had watching the Jetsons or the sense of adventure with Mr. Spock and Captain Kirk on Star Trek. Attempts to focus on the future often seem to come down on the “what’s to become of me/us” side of emotions rather than the upside view presented by Fleetwood Mac in their rousing anthem written by Christine McVie, “Don’t Stop Thinking About Tomorrow”. They advise us to give up bemoaning the past. Although they never quite say it, one assumes that a focus on the past is just too easy and leads to wallowing in the miseries of the moment.
It does not take advice from Fleetwood Mac for you to know that along with uncertainty, all the promise of something better lies in the future. Their advice is that if the past and the moment leave you hoping for more then “Don’t Stop Thinking About Tomorrow”. The lyrics say it all, “Yesterday’s gone…you’ll see things in a different way…It’ll be better than before…Why not think about times to come…Don’t stop, it’ll soon be here.”
During a presidential election year it is hard to think about the future without thinking the how the election will affect the future. Thinking about the future it is reasonable to wonder when the next recession will hit. We are eight years into a weak recovery and probably do not have the political consensus necessary to avoid another one in the next five or ten years, if not sooner. Will another recession eclipse a better future for healthcare by undermining an already vulnerable economy that has not recovered from its last near death experience? Despite our need to know there is little for certain that we can predict in terms of what the next recession will do to our efforts to achieve the Triple Aim other than the generalization that it will make it harder.
Out of all the uncertainty, what can we say that may be positive about how patients will experience care in the next decade? That is the question that put me into the hopeful space of “Don’t Stop Thinking About Tomorrow” and focused me on what I could say for sure about the experience of care in the future. I am assuming that we have the good fortune to experience slow but continuing economic growth, and I make the huge assumption that what has been gained with the ACA over the last eight years survives after the smoke settles in November. It’s not that I am just a Pollyanna, it’s more that I am like Christine McVie. So why not talk mostly about the upside possibilities of the moment for patients and realize that we have the opportunity to move into a better tomorrow?
I have spent the better part of fifty years thinking about what patients want and trying hard to figure out how to meet their expectations. Every patient is unique, but I believe that they hold many desires in common. The question is whether we will meet the expectations of more of our patients in the future. Patients have always wanted to be known. Beyond that desire for a relationship, at the core of what every patient and their family wants as they contemplate their care for the future, are two questions that need answers. First, will I have access to the care that I will need? Second, will I be able to afford the care I need?
The ACA has done a lot, but it has not answered either question. Much of what it has accomplished is taken for granted until a patient is exposed by personal experience to one of the problems it did correct, like the inability to buy insurance because of a pre existing condition. Many people who did not have care before are now covered, but many who once enjoyed almost free care now experience care that is more expensive than before. There has been a sort of “transfer” of benefit, as well as the taxpayer funded expansion of access. Some of us experienced a loss while others have enjoyed a much needed gain. I do not see this reality perpetuated into the future. Everyone needs a gain.
The finance of healthcare is in a metastable condition that must be resolved or at least mitigated. Those hurt the most, after we note that many still are denied care, are those in the broad middle class that carries a disproportionate share of the tax burden and now have increased copays and deductibles. The persistence of the healthcare finance problem also undermines our collective will and ability to use public dollars to chip away at other problems that are social determinants of poor health. It is a vicious cycle that requires an overall reduction in per capita spending while getting even more value for the dollars that we spend.
I am going out on a limb to say that in the next ten years our collective discomfort will force a political resolution or at least an improvement to the “cost” problem and eventually everyone will be covered at a cost that they find affordable. I believe that the patients who worry now about whether they can cover the expense of their care will eventually get at least as good an offering as the citizens of the “socialized” states of Western Europe. Really, if they can do it, why can’t we? We have a better overall economy and a huge vault full of cash called waste. We just need to find the combination to the lock on the vault to get at the resources we have that are currently out of our reach. I think it is possible, but it will not be easy.
The second issue of access will be easier because it will be not be a political issue. We will solve this one with our “go to– favorite” tools: competition, ingenuity and capitalism. We will effectively digitize healthcare enabling many “virtual touches” that will better leverage the professional capabilities of all clinicians. Patients have already demonstrated their desire for e-visits, televisits, group visits and alternative forms of care when it is obvious to them that the traditional methods of practice do not meet their access needs.
The vulnerable population to disruptive competition and innovation is not the public, but rather the providers who cling to outmoded workflows and continue to try to make patients walk through their fee for service turnstiles. All one needs to confirm this prediction is to go to any public place and sit and watch as people come and go getting advice and direction from their smartphones. Who knew what a “smartphone” was ten years ago? Medicine is slow to adapt but it will not be able to resist what happened to traditional retailers, taxi drivers, and motel operators. The healthcare equivalents of Amazon, Uber and AirBnB are already here and it is just a matter of time until all patients are using them. Some practices will get it and thrive and the others will go the way of Blockbuster. Patients will be delighted with their new, more efficient care with better access and convenience. Why waste time standing in the line at a pharmacy after waiting weeks for an appointment when your concerns can be resolved on line and your meds can be delivered to your mailbox? The concept has been proven and can be seen in leading practices.
There will be ways in which patients will benefit in the future that they may not appreciate. For the last 2500 years they have been vulnerable to the “art of medicine”. The art and intuition of medical experts is a source of error and much human suffering, despite the insistence of some that traditional medical practice should be treated like a religion. Doctors and nurses spending time with patients in an understanding and supportive way in therapeutic relationships will always be the core of practice. We stand in awe of what a caring clinician can do when supported well enough to spend as much time as it takes to give every patient what they need in a timely fashion.
The only way that it will be possible in the future for us to protect time and offer it to everyone who needs it by improving our work flows. With tools like Lean we will create the workflows that free up the time to provide the presense and time of the doctors, nurses, and other medical professionals at the right moment when there is the greatest possibility of benefit. The benefits of digital technology are going to eventually knock down or go around the barriers raised by those who call progress a “loss of clinical values”.
I see the patient of the future no more desirous of coming to the office for a BP check or advice managing their cholesterol or diabetes than they would be now using a telephone with a dial on it. Patients, through their demands, and those who pay for their care will eventually partner with clinicians and systems that care to co create the care that we will need in the future. I predict that the models of care and the ways that care will be delivered will make our current processes of care delivery look about as quaint and as out of date as approaching peptic ulcers with a bland diet, antacids and a gastrectomy.
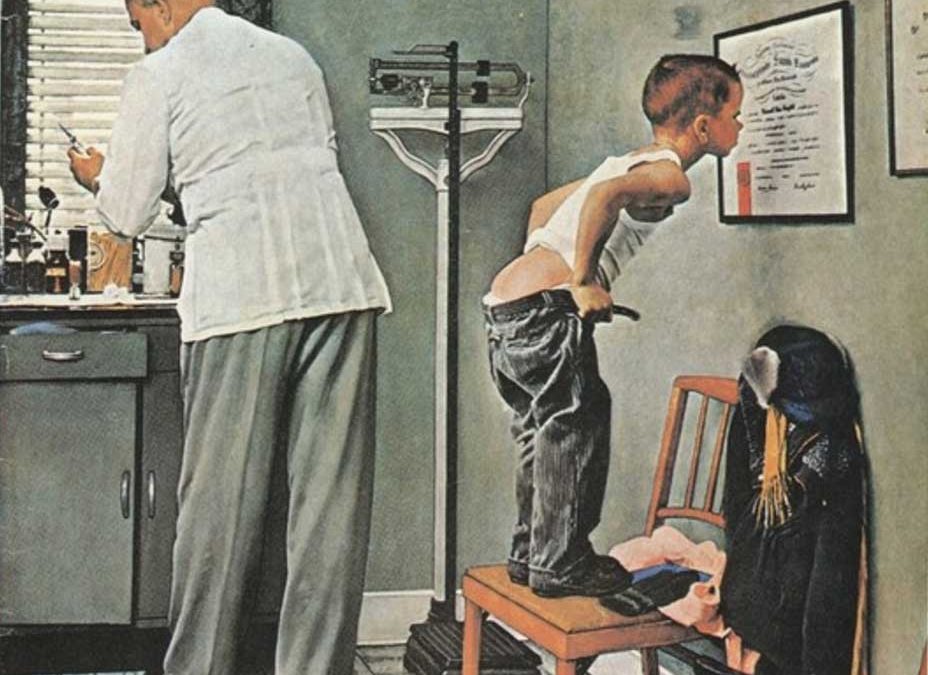
One of the things I enjoy the most these days is looking at innovations, high tech and low tech, and thinking back over the innovations that I have experienced in life, and realizing that progress in science and engineering has been geometric. We had no fiber optics; we had no echos; we had no CT scans or MRIs when Medicare was passed in 1965. We now have many more things to offer but their benefit and distribution are encumbered by our ineptitude with equitable distribution. We often can’t get what we have to those who need it, when they need it. Our failure arises in part because we still have the basic finance of 1965 and much of the medical mindset and culture of 1965. It is our finance, our preferred work flows, and perhaps in part, our nostalgia for an era when many had no coverage for care and depended “on the kindness of others”. The patient of tomorrow will get her questions answered or move on to see someone in a system of care that embraces the possible, even if that embrace requires some change and adaptation.
McVie had it right. Let’s not stop thinking about tomorrow. Tomorrow will be a better day when yesterday is gone. Patients will see things in a different way..It’ll be better than before…Why not think about times to come…Don’t stop, it’ll soon be here.”