Looking back over 2017 I am moved to say, “You can’t make this stuff up!” That expression is a meme/cliche that entered our culture sometime since the advent of Facebook. It has been used more and more during the evolving chaos of the first year of the Trump presidency in general, and specifically when tracking the fate of the ACA during 2017. Do you remember the drama of John McCain’s downturned thumb?
The saga of the ACA, or if you prefer, ObamaCare, has educated a growing number of people who are beginning to understand the principles upon which it is built, and are now willing fight to preserve them. We don’t have universal coverage yet, but more people now realize why we should. To our surprise and delight at the end of the year we have lost less ground to the ideals of universal coverage and the Triple Aim than we would have ever predicted after listening to the president’s inaugural address.
This time of year there are a lot of “year in review” articles and lists of “The Best___of 2017.” Number one on “The list of Best of 2017” articles from the Commonwealth Fund was their July offering “Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care.” It compares healthcare data from the top ten performing countries of the world with the performance of the United States. We rank behind Australia, Canada, France, Germany, The Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United Kingdom. Perhaps we would have ranked even lower if Japan or other EU countries like Denmark and Italy had been included. In a ranking of life expectancy alone we are in the high 20s, virtually tied with Cuba.
To the best of my memory, over this turbulent year while attacking the ACA, Republicans never addressed most of the deficiencies in our system in the domains that the paper reviews for its rankings:
- Care process
- Access
- Administrative efficiency
- Equity
- Health care outcomes
The results of the comparisons of performance in these categories are depicted below:
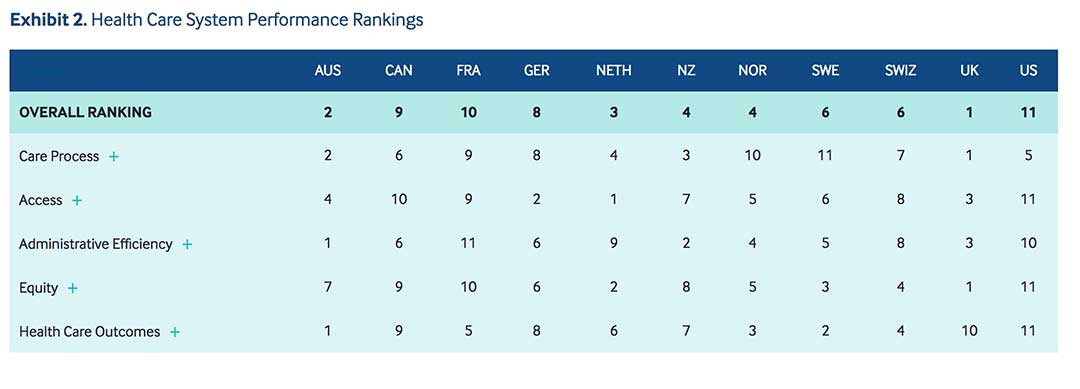
Accentuating the positive, we did best in the “Care Process” category where we ranked fifth. As described and measured, Care Process has four subdomains: preventive care, safe care, coordinated care, and engagement and patient preferences. The paper carefully describes what each subcategory includes, and how each one was measured. In my opinion, one reason we scored better in this category was the work of Don Berwick and the IHI who inspired our collective efforts to improve quality and safety through programs of continuous improvement. Despite disparaging slurs such as “Medical Taylorism,” I think the spread of Lean, which teaches “management by process” has contributed to improved “Care Process” where it has been given a chance by enlightened leaders.
The “government” efforts prior to January 20, 2017 were also success factors that pushed us to number five through the programs initiated by the ACA. There was surely benefit to our score in the “Care Process” category from the 40 billion dollars that the government invested in providing electronic medical records to physicians, and the follow up focus on “Meaningful Use.” The early efforts to move from “volume to value” based reimbursement in Medicare, Medicaid and some commercial products may also have contributed. The study looks at where we were prior to Trump’s election. Though limited, the success of these programs during the Obama presidency has been a good start, but now the government is controlled by those who favor reverting back toward the laissez faire attitudes that will propagate waste, expense, and poor outcomes for a growing number of Americans.
The only other category where we are not dead last was “administrative efficiency.” In this category four measures looked at barriers to care like difficulty getting a doctor, obtaining records and test results as well as the difficulties medical professionals have with administrative paperwork and payment delays. We love to talk about the deficiencies and delays in the UK, but that is mostly “fake news.” They actually rank number one in Care Process, Equity, and in the overall rankings! The rankings were done rigorously, and every country has room for improvement as demonstrated by the fact even though the UK was the gold medal winner overall, they were number ten in Health Outcomes, beating only us.
I accept the concept that equity is a human rights issue that impacts every aspect of quality and care delivery. I am surely biased, but believe that we compare poorly in the analysis of our nation’s health system’s performance to other developed nations because, unlike them, we have not taken the first step toward equity which is universal access. We all share the blame and consequences of long ago not more vociferously demanding equity as manifested minimally by universal access.
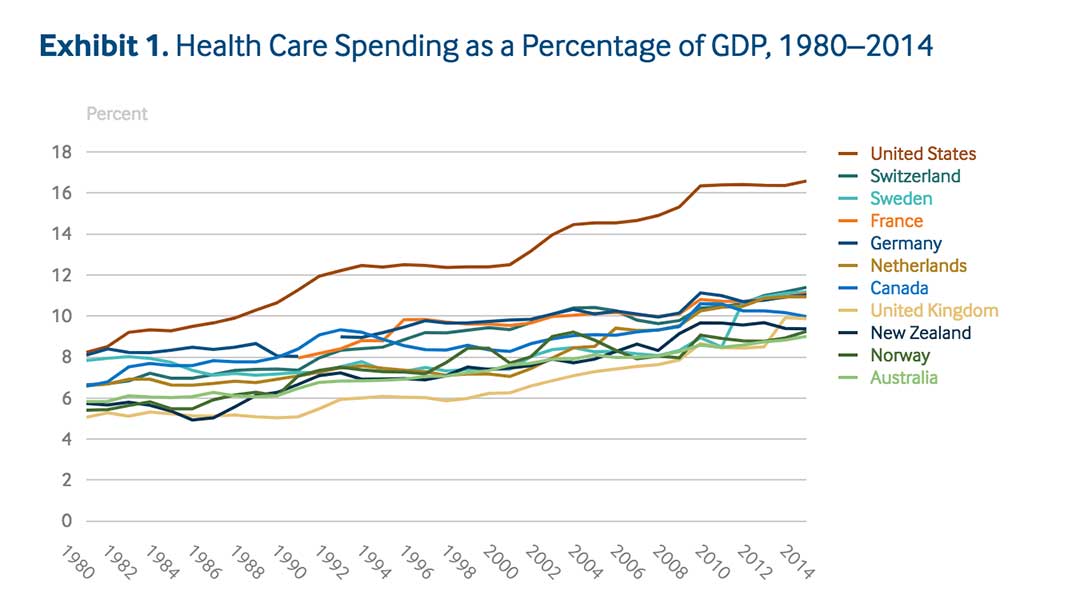
One of the things that has irked me since the inauguration last January has been how the Trump administration and the Republican majority in Congress have used the current costs in the self insured market as a political argument against the ACA. The irresponsible aspect of the political discussion is to point to the current situation and not do any analysis for why it exists. Our current health care cost dilemma took us at least 35 years to produce. Prior to 1980 our costs were not much different proportionately to the other ten nations in the Commonwealth Fund analysis.
If we were politically positioned to improve our metrics, we might benefit form a recent New England Journal of Medicine article, “Evidence-Based Health Policy” by Katherine Baicker, Ph.D., and Amitabh Chandra, Ph.D.. The piece describes how to responsibly and effectively incorporate the reams of data that are being produced in this digital age into effective policy decisions. Just knowing that costs are high and applying your bias to explain the reasons, and then jumping to a solution defies and desecrates the foundational concepts of continuous improvement. The authors point to three principles that need attention when trying to implement Evidence-Based Health Policy (EBHP).
- Policies need to be well-specified; a slogan is not sufficient.
- Implementing EBHP requires us to distinguish between policies and goals.
- EBHP requires evidence of the magnitude of the effects of the policy, and obtaining such evidence is an inherently empirical endeavor.
They underline the role of bias in political discussions about healthcare. Their point applies both to passionate seekers of the Triple Aim, like me, and those hoping to undermine and disable many entitlement programs.
In addition, just as the distinction between policies and goals is often muddied, interpretations of the evidence are often flavored by the implicit goals of the analyst.
They conclude with wisdom that could be interpreted as a call for attitudes that foster bipartisan policy efforts. Progress is dependent on finding common ground. That common ground must include agreement on shared values and goals:
But as important as evidence is to good policy choices, it can’t tell us what our goals should be — that’s a normative question of values and priorities. Better policy requires being both honest about our goals and clear-eyed about the evidence.
The ACA did not get implemented until 2014, and is not the cause our current cost problem. The ACA contains values and goals shared by most of the public and most healthcare professional that support the Triple Aim. I believe the Triple Aim describes goals that could be the common objective of the public and politicians. The Triple Aim recognizes economic sustainability as a core goal. My list and your list of what has created our cost issues that undermine sustainability would be an exercise in comparing our biases. What is an indisputable fact is that over the last 35 years our system of care has become more expensive without creating better outcomes than other advanced nations. We have different points of view about what has created our cost crisis, just like we have differing opinions about the causes for the weather we jointly experience.
My bias is that for several decades, rather than worrying about the cost of care, we have mostly focused on payment and market share. We are mostly driven, not by a desire to improve health, but by the pursuit of better bottom lines for individual practitioners and systems of care through as high a fee for service payment schedule as tolerable and have justified those high payments as necessary to create the resources to attract market share. We have falsely justified consolidation as a way of promoting efficiency and quality when we were really using it to control markets to institutional advantage.
The Commonwealth Fund article succinctly sums up much of what I have tried to say:
Based on a broadly inclusive set of performance metrics, we find that U.S. health care system performance ranks last among 11 high-income countries. The country’s performance shortcomings cross several domains of care including Access, Administrative Efficiency, Equity, and Health Care Outcomes. Only within the domain of Care Process is U.S. performance close to the 11-country average. These results are troubling because the U.S. has the highest per capita health expenditures of any country and devotes a larger percentage of its GDP to health care than any other country.
Their bottom line:
The U.S. health care system is unique in several respects. Most striking: it is the only high-income country lacking universal health insurance coverage.
Perhaps the most interesting point that the authors of the Commonwealth Fund paper make is that the ten countries that exceed our performance all have universal access. They get to their better results following different formulas for universal coverage. Analysis demonstrates that there are at least three mechanism of finance that work. The first ranked UK has the most “socialized” system. Most PCPs own their own practice but the hospitals are mostly owned and managed by the government, and most medical specialists and hospital based physicians are government employees. Regional councils manage the care of their populations to budgets and standards set by the government.
Australia, ranked second in overall performance, has a much less socialized system of care than the UK. It operates as a “Medicare for all” system, with the government paying the bill to private providers, but some patients “opt out” for private care. In a way, it is similar to American education with a mix of public and private school options.
Finally, the Dutch who rank third overall but are first in access, and second in equity, have a system that includes community rated premiums, managed competition with subsidies for the poor, and a mandate that everyone participate. It’s not all that different than the ACA tried to establish for us.
Looking forward, I do not see much happening in 2018 other than an election. Perhaps the erosion of the accomplishments by the Obama administration with the ACA is over. Perhaps we will limp forward toward better understanding of how to effectively achieve the Triple Aim with the hope that someday all the pain and suffering we have now, and will continue to have for a while, will end. Perhaps someday we will have the wisdom and the better experience of the Dutch, the Brits, or the Aussies. Between now and that time I encourage you to continue to work for something better globally, and to ask yourself on a daily basis what you can do locally within the current constraints to make things better. To be better a significant transformation is required at all levels. I contend, as I have for sometime, that to be better we need to put our personal and institutional concerns behind those of our patients, and in particular behind the concerns of the underserved who experience both medical neglect and economic inequities.
I do not like the “dog whistle” politics of “Make America Great Again,” but I sure would love it if in a few years the international rankings of healthcare showed us to be number one in all categories. For that dream to come true there is a lot of work to be done.