Last Friday’s Healthcare Musings began:
At four o’clock on Tuesday afternoon I was sitting at a table in the ballroom of the Boston Seaport Hotel at the 6th ATLAS (Annual Thought Leadership Symposium). This year’s conference title was “Expanding Boundaries. Removing Barriers.” I have attended all of the ATLAS conferences as a member of the Clinical Advisory Board of Kyruus, the company that sponsors the event, and I have written about several of them. The speaker at that moment, David Shore, an authority on change management and innovation, was the last of several exceptional speakers that included the famous former CEO of the Cleveland Clinic and ground breaking cardiovascular surgeon, Dr. Toby Cosgrove. Dr. Shore’s subject was “Leading Change With Actionable Strategies.” There had also been demonstrations, break out groups, and panel discussions that were focused on timely subjects that centered around effectively capturing the benefits of technology to transform care delivery. I had been at a banquet of ideas. I was trying to figure out how I was going to weave all of the ideas that I had heard into a meaningful presentation for you to read.
Then I got sidetracked with the implications of Nancy Pelosi’s decision to initiate an impeachment inquiry in the House of Representatives. I doubt that action needs more comment from me at this time. Some of you may think that it did not require any comment from me last Friday, and might have preferred another subject like the note I was thinking about writing when I got the notice of Speaker Pilosi’s imminent announcement. I finished my note with a promise:
Come back on Tuesday and I will tell you what I learned from Toby Cosgrove and David Shore at the ATLAS conference before my phone started to buzz.
I have had a week to mull over the experience I had at the ATLAS conference. I have not changed my impression. It was an exceptional experience, and deserves further comment. For several years now I have the same thread running through what I write. I have tried to articulate my concern several different ways. Perhaps the most succinct statement of my concern is “Stein’s Law”: “If something can’t go on forever, it won’t.”
If Stein’s law doesn’t seem to say anything about the future of healthcare to you let me explain the connection I see. I’ll begin with my favorite quote from Dr. Robert Ebert, the Dean of Harvard Medical School when I attended, and who founded the Harvard Community Health Plan (HCHP) fifty years ago in October 1969. That organization and its legacy practice, Harvard Vanguard Medical Associates, was where I spent my entire professional career. In 1965, while seeking funding for his idea that would become the very innovative HCHP, Ebert wrote:
The existing deficiencies in health care cannot be corrected simply by supplying more personnel, more facilities and more money. These problems can only be solved by organizing the personnel, facilities and financing into a conceptual framework and operating system that will provide optimally for the health needs of the population.
Dr. Ebert recognized over a half century ago that practice as we knew it, and care as we delivered it, was inadequate and unsustainable. It is clear from the quote that he would have been delighted to attend a conference that was billed as “Expanding Boundaries. Removing Barriers.” I must admit that it has surprised me that a system that is so expensive, so dysfunctional, so hard to navigate, so potentially dangerous to so many people, has survived for another half century. Perhaps it has survived because we have never forced it to be efficient. We have never demanded that it be of consistent safety and quality. We put up with delays in service, and we can only grumble if we can’t call an insider who is connected and can pull some strings for us and be our advocate when our access to the care we need will not occur in a timely way. We (I am a patient now) sit quietly and put up with the view of our doctor’s back and the apparent disrespect of a system that is focused on its own issues and usually gives only insincere lip service to the obvious alternative of focusing on the patient’s needs. Most egregiously, and the most significant reason that this can’t go on forever, and should not go on much longer, is that it is a system that lacks equity.
We are focused on the fact that there are 30 million people without coverage. We don’t worry much about those who are “covered” but still face huge medical bills if they seek to access care and therefore avoid care for fear of getting bills they can’t pay. As an aside, over the weekend I was the “KREM Steward” on call for the weekend. I fielded a call from a very distraught woman on Medicaid. She has a history of lupus and has had multiple hospitalizations. She is a single mother working hard for a little more than minimum wage. To my surprise her need for the financial assistance of KREM was because she is virtually penniless and has outstanding bills to Dartmouth Hitchcock Medical Center that Medicaid would not cover. Now she faces a new cancer diagnosis and is not sure how she will pay her rent or feed her daughter. I wanted to tell her things would be better after the next election. Something this bad can’t go on forever.
“Expanding Boundaries. Removing Barriers.” sounded like a meeting that might connect with my concerns. I was excited to hear Toby Cosgrove speak. As a cardiologist I was clued into his contributions to cardiac surgery. I have had a couple of friends and colleagues who traveled to Cleveland because he was the one person whom they wanted to open their heart and apply a fix. Early in my time as a CEO I had been in an adversarial conversation with him at a conference. I had also been a little surprised with reports that he might have been trying to get a position in the Trump administration, but recently there has been some interesting new information on the subject of why he did not become a member of the Trump cabinet.
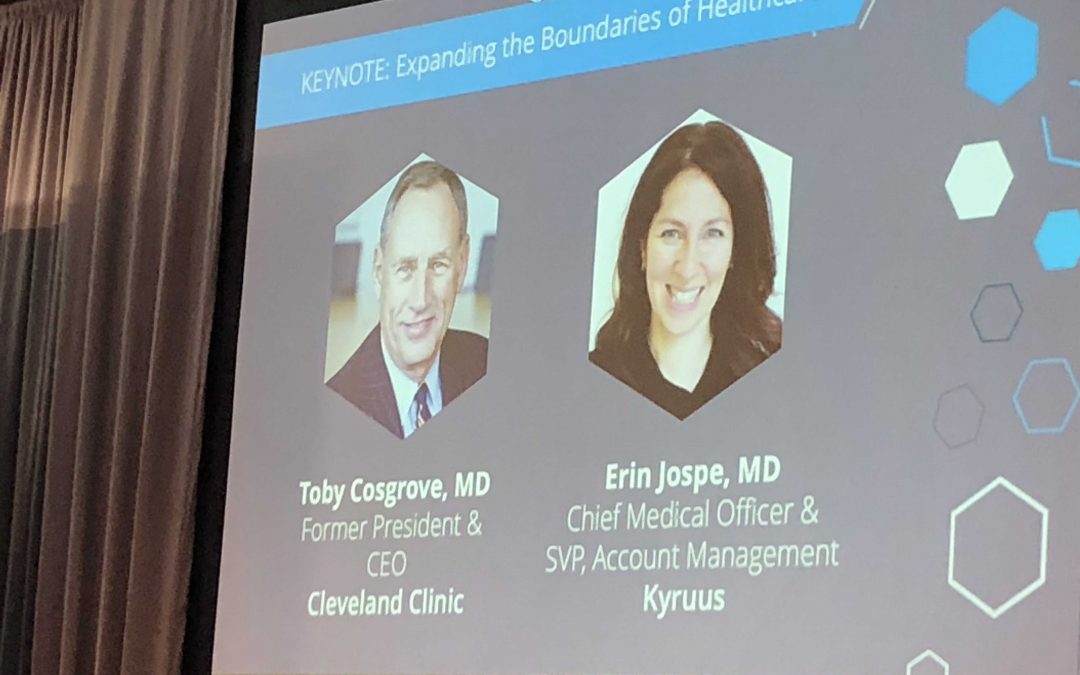
All these things were going through my head as I settled in to listening to Dr. Cosgrove’s “keynote address.” The first surprise was that I was not going to hear a speech or a lecture, but rather I would be listening to a conversation between Dr. Cosgrove and Dr. Erin Jospe, the CMO of Kyruus. I am a big fan of Dr. Jospe whom I first met when she was a PCP at the Post Office Square site of Harvard Vanguard/Atrius Health. She is a great conversationalist and a terrific leader. I thought, “Well, maybe this will be more interesting than I thought.”
The first thing that the conversation with Dr.Cosgrove revealed was that he won a Bronze Star in Vietnam in 1967 as an Air Force surgeon. Dr. Cosgrove is definitely an innovator. He holds many patents for devices that he has invented to improve cardiac surgery. He was the CEO of the Cleveland Clinic during a period of rapid expansion and transformation from 2004 through 2017. Starting then, and continuing now, Cleveland Clinic has expanded to other states and abroad. Here are some other facts and observations that Dr. Cosgrove offered during the conversation:
- True creativity exists at the boundaries between systems.
- Hospital organization has traditionally been an “extension of guilds.” Dr Cosgrove reorganized care at the Cleveland Clinic around patient problems.
- Success depends upon the performance of the “whole team.” That includes everyone, clinical and non clinical, who works at the Cleveland Clinic.
- Care was taken to ensure that the “culture” that was developed in Cleveland was transferred to every new practice site around America and the world.
- Maintaining the “culture” is the most important job of the CEO.
- Leadership is not a “technical job.” Cleveland Clinic takes people who are technically good and teaches them how to be effective leaders.
- People leave their organizations because they don’t like their managers.
- Why is healthcare so slow to adopt new ideas (13 years on average)? Because medical education does not promote searching for new ideas. It promotes looking for problems.
- “Patients First” is the “North Star” of the Cleveland Clinic.
- “Virtual Care” will be an enormous opportunity. 50% of Kaiser encounters now are virtual visits. Across the country neither doctors or patients have adjusted to the idea.
- We are “swimming” in data. Data in healthcare doubles every 72 days.
- Artificial Intelligence, Machine Learning, and the “Internet of Things” will define the future of healthcare. (Dr. Cosgrove is an adviser to Google.)
- Transparency is important. At Cleveland Clinic HCAP scores are published “in rank order by name.”
- All institutions will be under enormous financial pressure in the future. 62% of patients are on Medicare or Medicaid. The number of “no pay” is going up every year.
- We must move to more pay for “value” and reduce the cost of care.
- More care will be delivered in the home and in the ambulatory environment by “physician extenders.”
- Cleveland Clinic has a Chief Wellness Officer. A focus on wellness has reduced utilization.
- We don’t spend enough on social programs.
- In Ohio 50% of the state budget is for social programs.
- Team play is not a natural act for doctors.
- Cleveland Clinic doctors are compensated on the basis of the value they have added that is determined by an annual review, and not by RVUs, total billing, panel size, or number of procedures performed.
That’s twenty one statements that add up to the suggestion that Dr. Cosgrove would agree that what has been, will not go on forever. He is clear about the need for change and that he expects it soon.
On the second day the “keynote” presentation was by David Shore, “a leading authority on innovation and managing change initiatives to gain competitive advantage.” Again, I was an eager receiver of “pearls.” Dr. Shore did deliver a traditional presentation complete with slides and questions directed to the audience. It was during his presentation that I was distracted by the beeping on my phone that announced that Nancy Pelosi was about to have a press conference where she would initiate the inquiries that might result in the impeachment of Donald Trump.
Dr. Shore suggested that we always begin with the question, “Why are we having this conversation?” He went on to say that if we answered that question we might save ourselves from a lot of failure and frustration. He estimated that at least 70%, and perhaps 95%, of all “change efforts” fail. He followed up that fact with a disturbing observation, “First you shape your questions, then your questions shape you.” I needed to think about that one for a minute, but I think that is true. It suggests that if our questions are not the real questions of concern, our efforts to find the answers to our questions may become exercises in frustration. He continued his emphasis on the importance of asking questions by saying that workforce engagement is limited by the fear of asking questions. He then noted that questions are so important that progressive German companies have a new position, Direktor Grundsatzfragen, Director of Fundamental Questions.
He advised us not to “fall in love with our solutions,” and be sure to define “better.” He pointed out that the questions to answer were “Why aren’t we better? Why aren’t we happier?”
At this juncture I realize that he is describing a sold Lean approach. What is the reason for action? What is the current state? What would be better than the current state?
He then addressed the old wisdom that “culture eats strategy for lunch.” Transformation and cultural change are more difficult than they appear. There are cultures, subcultures, and countercultures in every organization. Strategy formation is a starting place. Implementation is what lies beyond strategy. Transformational change is resisted because of fear, because of the unknown. It is easy to derail a strategy by asking, “What are the unintended consequences?” People fear change even when it is for the good. An innovation must produce a positive change.
He moved on to discussing change by stating that in most groups the dominant attitude could be described by the acronym, CAVE. CAVE stands for consistently against virtually everything. It’s companion is ABC. ABC has been Anything But Change. It should be “applied behavioral change.”
Based on human nature he stated that change requires learning, and that no one learns in their “comfort zone.” They also don’t learn when they are terrified in the “panic zone.” Learning occurs in a zone of tolerable discomfort. He asserts that we have a higher success rate with change when it is gradual. True transformational change is rare. For change to occur the participants need to trust that if they fail they will still be safe.
That last comment brought me back to a core necessity for success with Lean. Participants in a Lean process need to trust that the process is about eliminating waste and improving a process, not about cutting jobs. I have written before about the necessity of “Relational Contracts” for success with Lean.
It was a good conference. It reinforced my bias that change is inevitable. Will the changes we experience over the next few years be a medical version of global warming? We do have an understanding of the changes in human behavior that would be necessary to save the planet, and we don’t seem to have the collective will to do what is necessary to change what we do to save our planet from disaster. Will we also fail to make positive changes in healthcare? Dr. Ebert’s call for change has been ineffective as a warning now for over 50 years. Remember, “If something can’t go on forever, it won’t.” We can’t survive in the world that we want to live in if the temp keeps rising. Likewise, we can’t have a system of care that delivers the Triple Aim objectives without change. Since “If something can’t go on forever, it won’t” is probably true, we face a choice. We must change in ways that improve all six domains of quality– patient centeredness, safety, efficiency, effectiveness, timeliness, and equity, or see the care process become increasingly expensive while meeting the needs of fewer and fewer people. In the end the system is threatened for everyone.
Dr. Cosgrove tells us that success depends on leadership and a positive culture, and Dr. Shore contends that implementation, more than strategy, is key to successful transformation. Positive transformation is not easy. It depends on leadership that can foster an environment of trust. I hope that a shared desire to avoid the consequences of a failed system of care will produce leaders, and a host of dedicated followers, with a desire to learn how to be better. We live in uncertain times where the reality that “if something can’t go on forever, it won’t’ can be either a promise or a threat. It is up to us to determine which one it will be.
The 6th ATLAS conference left me thinking that maybe, just maybe, we might someday find the answers that Dr. Ebert believed did exist. Dr. Cosgrove is right when he implies that the best way to find those answers is to realize that we must always be true to the “North Star” principle that we put patients first.