As we peer into the future and ponder what lies ahead for the practice of medicine we can be sure that the answer will vary across the spectrum of practice. To examine the potential changes for every type of practice would require a very extensive effort. If we focus on some of the high level issues that will be shared by all medical professionals then there is something to be learned.
I recently attended a performance of Cirque Du Soleil and was once again reminded of both the art and complexity involved in the practice of medicine. It was not my first time to attend one of these very remarkable presentations. Each visit has been an amazing experience. Every show is a different display of acrobatic skills, amazing costumes, dazzling sets, precision choreography, live music and thematic fantasy. Since 1980 there have been about thirty uniquely different presentations. Cirque Du Soleil has more than 9000 performers working around the world and earns about a billion dollars in revenue, most of which is consumed by their elaborate offerings to amazed customers.
David Brooks writes about the difference between the beautiful and the sublime. Brooks calls beauty that instills awe “big love” and say that it is sublime or transcendent. I was surprised to realize as I watched this remarkable evolution of the art form of the circus that although there was much beauty to appreciate in the performance, I was most moved and was awed by the ingenuity that brought it all together. Every performer was talented and taken individually they were entertaining, but it was their coordinated performance that was awe inspiring.
The evolution of the “circus” from a collection of remarkable independent acts and performances into one seamlessly coordinated physical, musical and visual experience seems to me to be a lot like the evolution of healthcare. In both, there have been real changes in presentation and possibility. In both, what you see is an outcome that is dependent on a tremendous amount of behind the scenes coordination. Workflows are executed with precision that always presents the action at the appropriate moment in the live music. There is the coordination of mechanized scenery and other equipment. It was not until I did a little research on Cirque Du Soleil’s evolution that I discovered yet another similarity to healthcare–finance. The greatest threat to their continuing performance has been the complexity of financing such a huge operations where there was never a secure return on investment.
The experience is dependent upon the actions of individual performers, and there are stars, but the awe and the impact comes not from the efforts of one but from the efforts of many who may be onstage, behind stage, or in some distant office. Does that sound like healthcare to you? It has not always been that way in medicine and it has not always been that way at the circus.
Today’s circus has radically changed how the show is developed and delivered. Now the performers blend their skills into something that presents its audience with an even more interesting experience. The challenge to all medical providers now is whether or not they can blend their offerings into a new effective systems of care with innovation providing creative new tools and workflows.
In Lean we talk about “a reason for action” and the current state as we imagine an improved or ideal state. Getting to the ideal state requires an analysis of the gaps or barriers between what is and what might be. The process allows the people who work in the system to propose and test paths to the improved state. Experiments, tests, and pilots, are proposed that might confirm solutions that were triggered by the reason for action and envisioned in the ideal or improved state. The cycle begins again after reflecting on what has been learned. As the songs says, “It’s often easier said than done!”. But the more you do it, the more you learn. I would be surprised if some sort of process of continuous improvement and learning is not a part of the success of Cirque Du Soleil.
For the last quarter century healthcare has been involved in one huge slowly moving improvement process. In the nineties we articulated our reason for action as care characterized by error, poor safety, high costs, and limited access. We began recognized that our delivery of care was designed around the convenience and financial needs and interests of individuals and institutions that provide professional services and not around the needs and concerns of the patient. We diagnosed ourselves as being inadequately “patient centered” with our self interests more of a daily driver than the safety, equity, timeliness, efficiency, or effectiveness of the care we were creating.
“Crossing the Quality Chasm” is about the progression from “current state” to ideal state. It began with a gap analysis and the description of the barriers to better care. I see Primary Care Medical Homes, “meaningful use” of EMRs, ACOs, bundled payments, the focus on population health and many innovations in care delivery as examples of the “experiments” to test partial solutions to our collective reason for action which is now articulated by many as the Triple Aim plus One. We have learned the importance of measurement, but we are still learning how to manage the intrusiveness of measurement. We are struggling as we integrate our need to measure with the practicalities of delivering care.
We are in the midst of a huge change process that will eventually improve the experience of practice for every clinician. No one individual or institution will be able to hide from, avoid or long resist the changes that have already begun as is evident every time you talk to anyone who delivers care. We are all being forced to consider changes that we would have never individually chosen or been able to consider, even though our previous and current results have demanded improvement. The personal impact that this has had on providers of care has been hard for everyone and devastating for many. If you really want to ruin the day of a physician, just inform them of the payment changes that are coming their way in the near future with MACRA and the need to pick a path, FFS, MIPS or APM into a future that they do not understand.
Before we envision the future let’s recognize the obvious and admit the existence of the current anger, fear, frustration and ultimate soul sucking burnout that is felt by so many people who chose a profession because it once offered the attractive dual opportunity of the joys of meaningful service to others and secure personal finances. Now most providers of care want to talk about their frustration and professional disappointment as they daily struggle with the endless tedium of practice laced with increasing regulations and the real risk of increasing financial vulnerability. The “chasm” that is referred to in “Crossing the Quality Chasm” is an abyss into which we have looked and into which many of us have fallen.
Last January I discussed Don Berwick’s proposed a path to a better future for practice that he presented in a wonderful keynote address at the IHI meeting in Orlando. You can view the entire speech on YouTube, but IHI also offers a neat seven minute video in which Don cuts the presentation down from fifty five minutes.
Don describes Era 1 as going back to Galen and the Greeks, like Hippocrates, and running up to sometime in the last thirty years. Much like the circus of the ‘50s, the workflows of practice and our clinical values did not change much over this very long period. During this era “Trust me, I am a doctor!” was not a joke. It was an expectation. Physicians had the ability to exercise their prerogative in all issues of patient care without much need for transparency or collaboration. Patients had no choice but to follow. The profession expanded the science of medicine and focused on mentoring successive generations of physicians to perpetuate its values.
Era 2 emerged in the 70s, 80s and 90s associated with HMOs, Medicare and Medicaid. Its focus was on accountability, measurement and “scrutiny”. Financial Incentives introduced “doubt” that could only be resolved with more measurement. No longer were physicians and caregivers explicitly trusted without documentation. Ronald Reagan famously said, “Trust, but verify!” That need to be accountable, measure performance, be scrutinized about potential fraud and abuse in a complicated system of incentives connected to performance, changed the relationship between providers and patients enjoyed in Era 1, and has brought us to the state of practice that is now bemoaned by so many clinicians.
Don’s Era 3 is the core of my prediction about what clinicians might look forward to as the foundation of a better practice experience. Don seeks to “harvest” and improve what was good from Eras 1 and 2 while jettisoning what no longer works or is now destructive. Don puts this all into one image that I have lifted as a screenshot from the seven minute presentation that I suggested that you review.
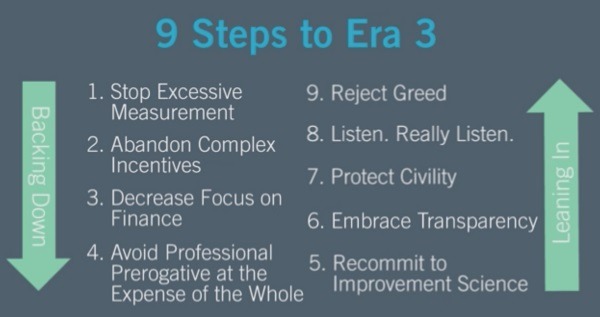
The focus on research, education, and values in Era 1 is foundational but we need to “avoid Professional Prerogative at the expense of the whole”. The issues in Era 2 require backing off from excessive measurement, discontinue complex compensation systems built off monetary incentives and give up the excessive focus on finance. Don suggests shifting the focus back toward mission from our obsession with finance.
Don’s ideas are more convincing as you study the “new” components of Era 3 on his up side of the image. By “committing to improvement science” we are shifting to a strategy of “efficient and effective, quality care” to maintain financial stability by taking less to do more. “Listen, Really Listen” is an admonition to put patients first. Don notes that the lack of respect that is so obvious these days in politics has also infected healthcare and we need to return to a more civil discourse as we work through the challenges of the future. Respect is the core concept of Lean. Finally, transparency is the antidote for a loss of trust and the need for excessive measurement to verify quality.
I see rapid movement toward a better future for practice. I talk to entrepreneurs in a variety of start ups and consultancies who are convinced that they can produce tools to support clinical performance and work flows that lessen the burden on clinicians and improve the experience of practice as they improve the experience of receiving care, all while lowering the cost of care and improving its quality.
As much as I enjoy the “art of practice”, when my time comes to need complex care I would prefer algorithms and workflows applied to my care that are driven by big data and the knowledge of the best practices that have worked over the faulty memory and limited data base of the most experienced and renowned practitioners of the art of medicine. It is hopeful to know that we need no longer to base management decisions in clinical practice on random recent experience, opinions from experts and the frailty of unsupported human judgement.
A great doctor with great tools working in an environment that has been engineered for her needs and the needs of her patients is the positive view of the future that both clinicians and patients can share. I hope that in the future the “art of medicine” will be employed to better “know” the patient as an individual and manage ambiguity when information is not available. We should embrace and celebrate our ability to articulate and evolve consensus around “best practices”. Within the next decade we should make huge progress in the direction of the “Triple Aim plus One”. With improvement in the experience of practice we will have
Care better than we’ve seen, health better than we’ve ever known, cost we can afford…for every person, every time.


