I recently accompanied Dr. Rushika Fernandopulle on a visit to the Iora practice site in Hanover, New Hampshire which was created in partnership with Dartmouth College, King Arthur Flour (an employee owned company) , and the New England Carpenters Health Benefits Fund. The Hanover site opened in March 2012, a little over a year after the New Yorker article by Atul Gawande that introduced so many of us to Dr. Fernandopulle.
I have been impressed with the similarity of Iora’s methodology and Dr. Robert Ebert’s thinking when he established Harvard Community Health Plan in 1969. On the Internet I discovered that like Dr. Ebert, Dr. Fernandopulle encountered significant resistance from the status quo. Ironically, for Iora the resisting status quo was Harvard Pilgrim Health Care! There is an article about this resistance from Boston.com writen in 2005 when Dr. Fernandopulle’s forerunner to Iora, Renaissance Health, was fighting to establish itself. In the article Dr. Fernandopulle defended the innovative practice:
For the past several years, I have worked on a project to create a radically better model of care. A model that would result in both increased healthcare quality and decreased costs. Based on research conducted through the Harvard Interfaculty Program for Health Systems Improvement, we have built an innovative primary care practice called Renaissance Health located on the Arlington/Cambridge border. By leveraging the most advanced information technology, empowering patients to play a much bigger role in their own care, and changing our paradigm of care delivery, we are building a new model to deliver better and more affordable healthcare.
Whether or not my visit to Iora’s Dartmouth practice would support my hypothesis that Iora and HCHP faced similar barriers, I hoped that the visit would open my eyes to a greater understanding of what Iora was doing and the barriers that stood between its current state and its vision. I met Dr. Fernandopulle at 7 AM. Over coffee he described his journey from the idea of being a surgeon when he was a Harvard Medical student to a residency in medicine at the MGH and a Master’s Degree in Public Policy at Harvard’s Kennedy School. He became Executive Director of the Harvard Interfaculty Program for Health Systems Improvement after he had spent some time at the Advisory Board Company.
From his position at Harvard, he attempted his first effort at innovation by building a new primary care practice called Renaissance Health. It was there that he introduced a new position called “care partners” now called “health coaches”. The idea was the product of observations that he had made on a mission to the Dominican Republic.
As his story unfolded it was obvious that he had remained true to his intent to “create a radically better model of care”. His intense focus on this vision seemed as genuine as Dr. Ebert’s focus on mission and vision. Each step in his evolution as an innovator had been a combination of learning from the previous step and an ability to add to the idea through collaborations that were offered because of his extraordinary ability to attract and engage interesting and talented people.
Iora’s success has been facilitated by collaboration with business partners that can see that their responsibility to provide medical care for a specific population can benefit from a partnership with Iora’s prepaid, no copay, focus on effective primary care that reduces total medical expense. Rushika told me that Dartmouth Health Connect was launched when Dr. Jim Yong Kim who was formerly at Harvard Medical School was Dartmouth’s President. Dr. Kim wanted an innovative practice to test ideas developed at the Dartmouth Institute.
As the conversation with Dartmouth evolved Dr Fernandopulle was able to recruit Dr. Joel Lazar, who was the Section Chief of Family Medicine at Dartmouth Hitchcock, to become Iora’s local leader. Just like the early resistance to Harvard Community Health Plan not everyone in the community was delighted with the idea of Iora coming to Dartmouth. One blogger bluntly asked whether it would be just a “concierge practice for the healthy” much like some of the detractors of HCHP who described that attempt at innovation as Horrible Care for Healthy People.
You can take a tour Dartmouth Health Connect online. When we arrived we were met by Robin Rice-Voight, RN who is the practice administrator and with Dr. Lazar forms the leadership “dyad” (my term not theirs) for the practice. Everyone in the practice meets at the start of each day for a “huddle”. I realized that Iora was utilizing aspects of “Management for Daily Improvement” and ‘Visual Management” as well as demonstrating the philosophy that everyone is a contributor to the care and everyone needs to be informed in the process of collaborative care.
The Health Coaches take turns in rotation leading the morning meeting. You can see the room on the Internet tour if you clicked on the link above. Two large screens were connected to a program in Google Drive that was the guide for the meeting and where data was entered for later reference by the team. The medical record and the various IT tools for practice have been largely developed by the staff utilizing Google Drive which allows the clinicians to create and modify what works for them before the tools are finalized as part of the IT platform of Iora.
You can view all of the bios of the team and appreciate how the position of Health Coach is open to anyone who is interested in people and service. There is standardized training, but I had the impression that much like the training of physicians in the hospital, the most effective learning occurs as work is being done in collaboration with more experienced professionals.
During the meeting all of the calls, admissions, discharges, transfers, and interactions of the weekend were reviewed. There was consideration of the work ahead for the day. Everyone works with everyone. Each of the coaches has a tight relationship with about 350 to 400 individual patients. Patients connect with the practice and their coach in the way most comfortable to them. “Chirp”, their collaborative medical record and patient portal, facilitates communication between coaches, physicians, and patients who can “chirp” with their team and contribute “data” that is important to them including their weight, blood sugar and blood pressure.
The team meeting agenda included “The Department of Small (and absolutely awesome) Victories”. Everyone enjoyed offering celebrations about patients who had reached some threshold of engagement or informing their colleagues about some project completed through collaboration. As I witnessed the enthusiastic exchanges among this group of teammates it occurred to me that it was highly unlikely that burnout or a sense of isolation would ever be a threat. I wondered, based on my experience with the stress of growth, if there were safeguards in place to protect this fragile ecosystem from the stress associated with the need to grow.
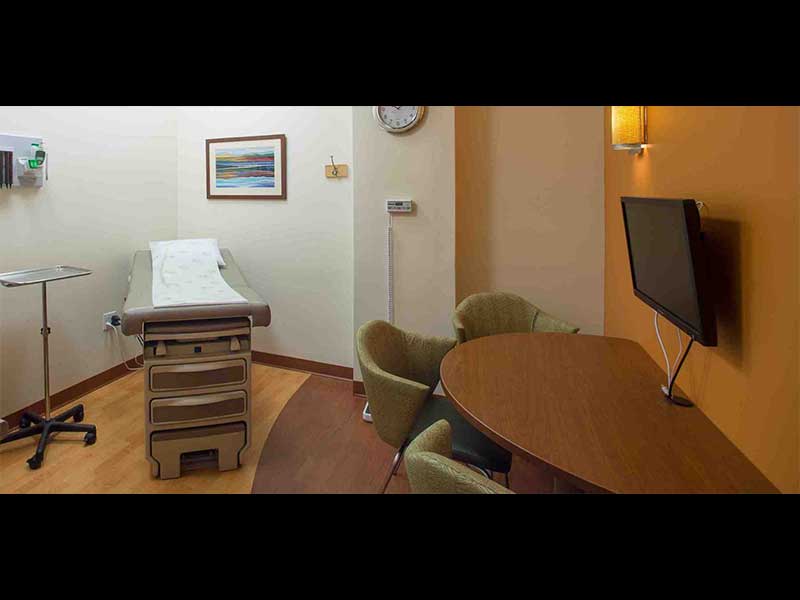
The group broke up to go to see their patients, make calls, answer emails, and continue case discussions between physicians and coaches. My first reaction was that from this point on “this is just nuts and bolts” primary care. I was wrong. Just looking into an exam room revealed an insight. There is a large computer screen on the wall with a semicircular desk with three chairs in front of the screen. The patient, the patient’s coach, and the doctor look at the data together. Today’s header shows the setup. If your objective is to pump as many patients as possible through your practice every day, then this would look like a barrier. If your belief is that patient engagement enables people to be healthier, and that healthier people use and need fewer expensive medical resources and have better outcomes, then this is an improvement that is a “least waste way” to provide primary care.
After checking out the exam rooms I began to observe patient flow and schedules. Visits were scheduled for thirty minutes or an hour and the first person to see the patient was the coach. After the use of Health Coaches, a second most obvious part of the Iora methodology is the focus on behavioral health. The PHQ 2, PHQ 9 and the GAD 7 are used almost as often as a stethoscope. The embedded social worker, is available for immediate engagement and consultation.
Dr. Laura Duncan and Gabe Wegner, the health coach who had led the meeting, allowed me to sit in on their conversation about shared patients. They continued a conversation that began in the morning meeting: how best to inform one of their patients who had a breast biopsy at a local hospital that the pathology revealed a cancer. It was decided that Laura would find out what the physician who had done the biopsy had communicated to the patient. After learning as much as possible they would offer an appointment to her and her family that day.
I felt that this was a “causeway” event. As long as care was provided within the environment that they controlled it was easy to stay in flow and optimize the patient’s experience. Care that needs to be acquired “across the causeway” with specialists or with hospitals requires extra work by the coach and clinician if Iora is to maintain the patient experience that is their goal.
The biopsy had been done the previous week in a community hospital and locating the doctor was not easy. It took a few calls to learn where the doctor was doing her business on this Monday and then more time to find out what that physician might have done or said about the results. The whole process took up a significant amount of Dr. Duncan’s time as she made multiple calls to find the doctor and learn what had happened. This is a problem that many PCPs face and establishing more efficient “causeway connections” must be on the “build list” for Iora.
Laura and Gabe knew the patient would know the biopsy was a concern when they called so their strategy was to bring the patient in as soon as possible. Improvising when the process of care with outside suppliers has not been established is a common source of wasted time in primary care and a contribution to economic waste across the country. It will be interesting to see as Iora grows how it builds the reliable bridges that its patients need.
Even within the famous AMCs and medical systems in Boston where all care comes from the same enterprise there is plenty of opportunity for improvement in communication between “silos”. Iora has done well to abolish its internal silos. Now Laura and Gabe were facing the well defended silos of the outside world.
Their phone conversation with their patient was a wonderful demonstration of empathy and respect. They put the patient first and made a series of calls that connected the patient back to them and Iora. I had departed before the visit but can imagine that “humanity was restored” once care was back within the practice.
When I just stood in the middle of the practice and watched what was happening, I was impressed that underlying the continuous collaboration was a palpable respect that you could hear and see in every interaction. I noticed that part of the corporate paraphernalia lying around was a small squeezable rubber cube. On each face of the cube there was corporate lingo that had been imprinted when the cube was created.
- Demonstrate Courage
- Feel Empathy
- Bring Creativity
- Act with Passion
- Serve with Humility
The sixth face had the corporate line “Restoring Humanity to Healthcare” and the other five faces were obviously components of that objective. Then I saw that someone who worked in the practice had inked in “Embody Hospitality” on the face of the cube that said “Restoring Humanity to Healthcare”. It was just another indication that Dr. Fernandopulle has launched an innovation that we should all continue to watch.